In clinics from Boston to Los Angeles, a quiet surge is reshaping everyday life: more urban Americans are reacting to the animals they love. Physicians are reporting fuller waiting rooms each spring and fall, and apartment dwellers say a short elevator ride can trigger a day of wheezing. The mystery is sticky, literally – pet allergens are microscopic proteins that cling to clothing, carpets, and air currents, evading quick fixes and easy blame. Scientists now argue it isn’t one culprit but a crowded team: denser living, tighter buildings, warmer seasons, and stressed immune systems all nudging sensitivities higher. The story is less about fragile people and more about environments changing faster than our bodies can keep up.
The Hidden Clues

Here’s the hook: even homes without pets often test positive for cat and dog allergens, carried in on coats, backpacks, and bus seats. That means city life becomes a shared exposure experiment, where the neighbor’s tabby silently travels the block on your hoodie. In my own reporting notebook, I’ve scribbled the same pattern in different ZIP codes – new symptoms after a move, worse symptoms after a heat wave, and sudden relief after a building’s filtration upgrade. Researchers point to the “stickiness” of certain animal proteins that ride dust particles and linger for weeks. It’s a story told by objects – doormats, couches, subway poles – more than by the animals themselves.
When you line up the clues, a pattern emerges that’s less dramatic than a plot twist and more relentless than a drumbeat. Multifamily buildings concentrate allergen reservoirs, while busy transit and shared laundry rooms amplify spread. Weekend cleanups help, but the dust rebounds by Monday morning. The better our insulation, the easier it is for indoor irritants to accumulate. The city, in short, is an allergen network, and each surface is a transfer station.
Urban Homes, Furry Friends

Pet ownership has climbed in recent years, and cities are no exception; parks brim with dogs at dawn, and cats rule high-rise windowsills at dusk. As more people spend time indoors – remote work, streaming nights, long winters in efficient buildings – exposures add up. Urban units are smaller, so each square foot must handle more dander, shed skin, and saliva-coated fur. Building materials and soft furnishings act like allergen sponges that are rarely rinsed fully clean. Even conscientious grooming can’t erase the fact that allergens are tiny and persistent.
Shared spaces add another layer that’s easy to overlook until symptoms show up. Hallway carpets, HVAC ducts, and package rooms can circulate pet proteins far beyond any one front door. Pet-friendly policies are a joy for residents and a challenge for their immune systems, because allergens don’t respect lease lines. I’ve heard from tenants who never met the neighbor’s dog yet felt the effects every time the central fan kicked on. In dense housing, the thermostat can be as influential as the leash.
The Science of Sensitization

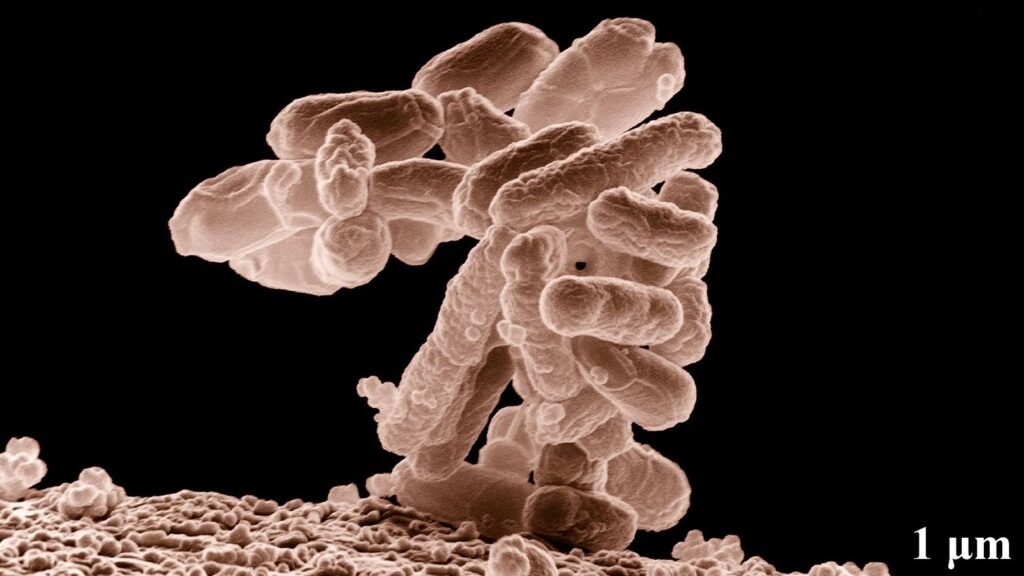
Allergies are a learning problem – the immune system studies a protein and, in some people, mislabels it as a threat. With repeated exposure, the body builds a quick-trigger response that releases histamine and other chemicals, leading to congestion, itchy eyes, or a tight chest. Certain pet allergens, like the dominant cat protein produced in salivary and skin glands, are particularly airborne and stubborn. These proteins latch onto tiny dust particles that stay suspended longer in dry indoor air, making each breath a small lottery ticket for sensitization. Add a compromised skin or airway barrier – think winter dryness or a lingering cold – and the odds tilt further.
Early-life timing matters, but it isn’t destiny. Some infants around pets develop tolerance, while others with eczema or a family history of allergy become sensitized faster. Urban pollutants and respiratory infections can act like amplifiers, turning mild exposures into teachable moments the immune system sadly remembers. Once sensitized, people can react in pet-free environments because the proteins travel so easily. It’s a memory that follows you on the subway and into the office.
Air, Heat, and the Microbiome

City air does more than obscure skylines; it primes inflamed airways that are quicker to overreact. Fine particles and ozone irritate the lining of the nose and lungs, lowering the threshold for allergic responses to pet proteins. Urban heat islands keep nights warmer, drying indoor air and helping allergens stay airborne and active. Climate change nudges this along by stretching warm seasons and altering humidity patterns that affect dust mites and indoor molds, both of which can team up with pet allergens to worsen symptoms. These are small nudges, but together they push the immune system toward a hair-trigger state.
There’s also the microbial story – the bacteria and fungi we cohabitate with – and it’s changing. People in dense urban settings often encounter less environmental diversity than those in rural, farm, or coastal environments. That reduced variety may leave immune systems undertrained and more likely to overreact to harmless proteins. Think of it like a guard dog with too little socialization: jumpy, loud, and quick to misread intentions. Cities need microbial variety as much as they need green space and clean air.
From Ancient Tools to Modern Science
Allergy testing has evolved from simple skin-prick trials to sophisticated blood assays that pinpoint the exact pet proteins involved. Component-resolved diagnostics now distinguish between major cat and dog molecules, helping clinicians tailor advice and treatment. Environmental testing is getting smarter, too – dust sampling, wearable air monitors, and building sensors can map how allergens move through a home. I’ve watched technicians vacuum a single square meter of carpet and learn more than a week of diaries ever revealed. Data from these tools is rewriting floor plans, showing where allergens pool and which interventions actually stick.
On the treatment side, standard therapies still matter – nasal steroids, antihistamines, and immunotherapy for carefully selected patients. But city-specific strategies are gaining traction: staged cleaning protocols, upgraded filtration, and targeted room-by-room plans. Even pet-care routines are being tweaked, from bathing schedules to grooming locations that minimize spread. The message is subtle but powerful: the right combination matters more than any one silver bullet. Precision, not perfection, is the new north star.
Why It Matters

This isn’t just about sneezes; it’s about daily function, household budgets, and public health. Allergic disease drives missed workdays, lower school performance, and more emergency visits for asthma in vulnerable communities. Tenants in older buildings can be hit harder by leaky ducts and aging carpets, while the cost of frequent cleaning and filters piles up. Pets also offer profound emotional support, so asking families to rehome them carries a heavy mental-health toll. The real win is reducing symptoms without sacrificing companionship.
Consider the practical stakes that ripple well beyond runny noses:
- About 70% of U.S. households include a pet, so small risk shifts affect millions of people.
- In dense housing, shared HVAC can spread allergens between apartments, raising exposure even for pet-free families.
- Asthma exacerbations tied to indoor allergens drive costly urgent care visits, especially during hot, stagnant weeks.
The old advice often boiled down to avoidance; the new playbook blends engineering fixes, medical care, and smarter habits. That shift matters for equity, because well-targeted environmental changes can deliver relief at building scale. When symptoms fall, attendance rises, sleep improves, and households regain momentum. Health, in other words, becomes a community project.
The Future Landscape

Emerging science is moving on multiple fronts at once. Researchers are studying vaccines and biologics that target dominant cat allergens, while novel diets and grooming products aim to reduce allergen levels at the source. Building standards are following suit, with momentum for higher MERV-rated filters, balanced ventilation, and sensors that flag stale, particle-heavy air. Real-time allergen detection remains a challenge, but pilot devices are starting to translate dust into data. Pair those with machine learning and you get a map of when and where exposures spike, down to the hour.
Urban design will quietly shape outcomes, too. Cooler, greener neighborhoods trap less heat, cutting the stagnant indoor conditions that let allergens linger. Landlords and co-ops are beginning to see filtration upgrades as investments rather than luxuries, much like weatherproofing a decade ago. Telehealth can broaden access to allergy specialists for renters who rarely have flexible schedules. None of this is flashy, but added together, it’s a blueprint for calmer air and calmer immune systems.
Conclusion

Start small and be consistent. Keep pets out of bedrooms, use allergen-impermeable covers, and run a high-quality HEPA purifier where you spend the most time. Vacuum with a sealed HEPA machine twice weekly, and wash pet bedding on a hot cycle to disrupt the constant resupply of proteins. Upgrade to a MERV-13 or better filter if your HVAC allows it, and change it on schedule, not when symptoms flare. If you’re symptomatic, talk with an allergy specialist about testing and, where appropriate, immunotherapy.
Think beyond your front door. Ask building managers about duct cleaning, corridor carpets, and filter maintenance schedules. Coordinate pet-grooming areas and ventilation so dander isn’t shared by the whole floor. If you can, support local initiatives that improve air quality and cool heat islands; cleaner outdoor air translates to calmer indoor air. Relief rarely comes from one move – it’s the stack of better choices that turns the tide.

Suhail Ahmed is a passionate digital professional and nature enthusiast with over 8 years of experience in content strategy, SEO, web development, and digital operations. Alongside his freelance journey, Suhail actively contributes to nature and wildlife platforms like Discover Wildlife, where he channels his curiosity for the planet into engaging, educational storytelling.
With a strong background in managing digital ecosystems — from ecommerce stores and WordPress websites to social media and automation — Suhail merges technical precision with creative insight. His content reflects a rare balance: SEO-friendly yet deeply human, data-informed yet emotionally resonant.
Driven by a love for discovery and storytelling, Suhail believes in using digital platforms to amplify causes that matter — especially those protecting Earth’s biodiversity and inspiring sustainable living. Whether he’s managing online projects or crafting wildlife content, his goal remains the same: to inform, inspire, and leave a positive digital footprint.