In the steamy Gulf air, where dusk hums with mosquitoes, a quiet threat moves from swamp to backyard, from bayou to porch. Heartworm disease isn’t new to veterinarians in Louisiana, but the scale and relentlessness of infections here keep rewriting the record books. The state sits at the center of a natural laboratory where climate, ecology, and human routines collide, and the parasite thrives. The puzzle is part biology, part geography, and part human behavior – and the stakes are measured in coughing dogs, breathless cats, and costly treatments. The story is not just about risk; it’s about how to outsmart a parasite that has learned to use the terrain to its advantage.
The Hidden Clues

Ask a vet in New Orleans or Lafayette what month is “heartworm season,” and you’ll get a tired smile: it never really stops. The hints are everywhere if you know how to read them – positive antigen tests arriving in clumps after heavy rain, microfilariae seen under a microscope like tiny punctuation on a lab slide, owners surprised that a mostly indoor pet could still be vulnerable. I remember stepping out of a Baton Rouge clinic one muggy evening and feeling the mosquitoes gather at the doorlight like iron filings to a magnet; it felt like the local ecosystem narrating the story for me.
Those lab clues echo a larger pattern: Louisiana consistently tops national maps for heartworm prevalence across dogs and cats. Warm temperatures speed mosquito development and shorten the parasite’s journey inside the insect, making transmission efficient and persistent. Add in long, wet seasons and abundant breeding sites, and the result is a conveyor belt for infection. The evidence paints a simple arc – mosquitoes are the delivery system, the climate is the accelerator, and pets are the unintended audience.
A Perfect Storm of Mosquitoes

Louisiana’s climate stacks the deck. Extended warmth keeps mosquitoes active for much of the year, and humidity supercharges their life cycle like a greenhouse for wings. Storms leave behind standing water from roadside ditches to hidden gutter seams, each a tiny nursery. Urban heat islands stretch the season even longer in cities, while coastal marshes serve as vast mosquito factories on windy summer nights.
It’s not just the numbers; it’s the diversity. Multiple mosquito genera can transmit heartworm, and some thrive in containers, some in floodwater, and others in permanent marsh. When one species dips, another steps in, keeping the transmission chain resilient. The state’s patchwork of wetlands, neighborhoods, and farm edges builds a relay team of vectors that rarely drops the baton.
The Parasite’s Playbook
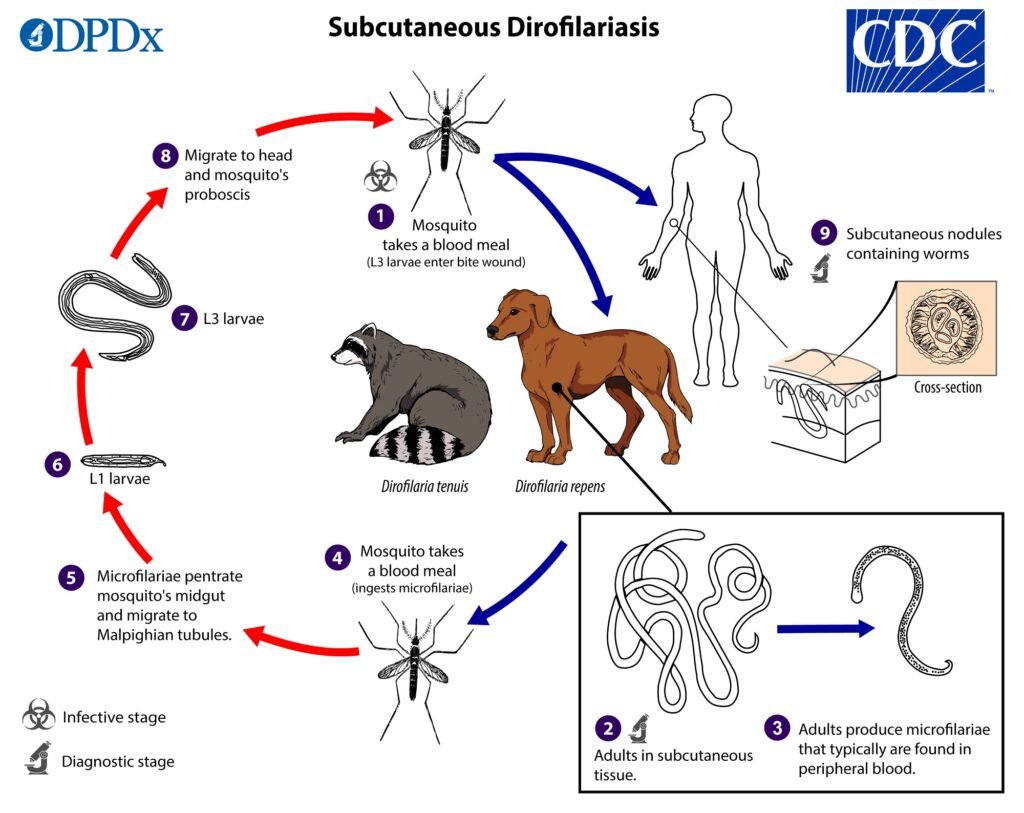
The Parasite’s Playbook (image credits: Wikimedia)
Dirofilaria immitis, the heartworm, is a strategist using micro-scale timing to master a macro-scale landscape. Microfilariae circulate in an infected pet’s bloodstream, then hitch a ride when a mosquito feeds. Inside the mosquito, larvae develop to an infective stage and migrate to the insect’s mouthparts, ready for handoff during the next blood meal. Warmth speeds that timeline, which means Louisiana’s heat cuts delays and boosts efficiency.
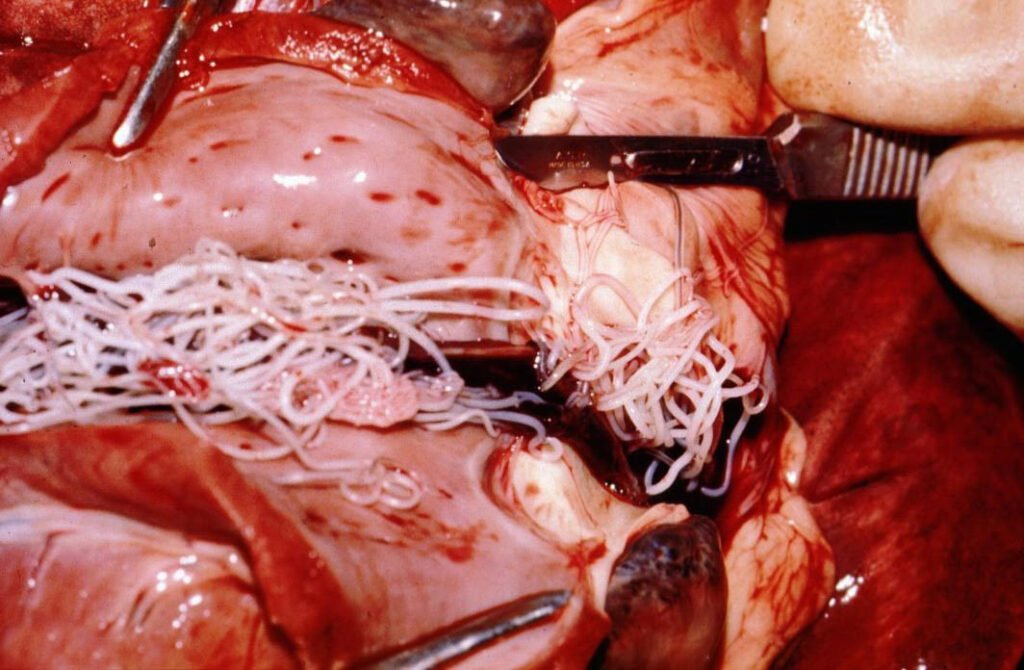
Once delivered to a new host, larvae settle in and mature into adults that occupy the pulmonary arteries and, in heavy infections, the right side of the heart. Dogs can harbor multiple adult worms for years, quietly building damage that shows up as coughing, exercise intolerance, and heart strain. Cats mount a dramatic inflammatory response that can resemble asthma, with sudden respiratory distress despite few adult worms. The parasite doesn’t need a large footprint to cause outsized harm, and that’s part of its power here.
People, Pets, and the Wild Edge

Human routines complete the map. Monthly preventives get missed during hectic seasons or after hurricanes, when priorities shift and supply chains wobble. Outdoor pets spend twilight hours where mosquitoes are thick, while indoor pets are assumed safe until one sneaks in through a door left ajar. Cost and access shape decisions, and in high-risk areas, even short gaps in prevention can be costly.
The landscape blurs the boundary between backyards and wild corridors. Stray and shelter populations serve as reservoirs, and post-storm displacement moves untreated animals across parish lines. Wildlife – like coyotes and foxes – can participate in the cycle at the edges of towns, ensuring the parasite never runs out of hosts. In this mix, prevention is not just an individual choice; it becomes a community-level intervention.
Why It Matters
Why It Matters (image credits: Wikimedia)
Heartworm is not a niche disease in Louisiana; it is a chronic pressure on pet health and on household budgets. Treatment for dogs is lengthy and expensive, requiring staged care that curbs activity and carries its own risks, while cats often can’t be treated the same way at all. Delayed diagnosis means more advanced damage to lungs and heart, turning a preventable problem into a life-altering one. In clinics, the emotional toll is real – decisions get made under strain when prevention lapses meet a positive test.
There’s also a wider scientific concern: there are concerns about potential reduced susceptibility to common heartworm preventives in some areas of the Lower Mississippi River Valley. That doesn’t mean preventives fail across the board; it means careful dosing, adherence, and integrated strategies matter more than ever. When a parasite gets more chances to circulate, evolution gets more chances to experiment. Louisiana’s high transmission pressure is exactly the scenario where vigilance is essential.
From Ancient Tools to Modern Science

Diagnostics have evolved from simple blood smears to antigen tests that pick up adult female worms, with confirmatory microfilaria checks to catch hidden infections. In cats, antibody and antigen testing paired with imaging helps untangle complex respiratory signs that can mask heartworm. Many veterinarians in Louisiana recommend annual testing even for pets on prevention, because real life includes missed doses, vomited pills, and unknown exposures. The goal is to shorten the window between infection and action.
On the prevention side, modern options include monthly oral or topical macrocyclic lactones for dogs and cats, plus long-acting injectable moxidectin for dogs that can cover a full year. Vector control – yard cleanup, screens, and repellents approved by a veterinarian – adds another layer, especially during peak mosquito hours. For positive dogs, a staged protocol using adulticide therapy, exercise restriction, and microfilaria management aims to clear infection safely. In cats, supportive care and prevention remain the core of protection.
The Future Landscape

Climate projections point to longer warm seasons and more intense rainfall events across the Gulf, magnifying the mosquito margin. That means the heartworm calendar stretches, and the number of infectious mosquito days grows. Forecasting tools that combine weather, land use, and diagnostic data are already guiding veterinarians to prepare for spikes before they happen. In Louisiana, that kind of early warning is less luxury and more daily necessity.
New strategies are under study: improved long-acting preventives, refined diagnostics that detect infections sooner, and targeted use of companion therapies like antibiotics against endosymbionts that support worm biology. Community-wide approaches – spay-neuter initiatives, post-storm mobile clinics, and shelter partnerships – multiply the impact of individual prevention. If the state leans on data-informed mosquito control and consistent preventive coverage, the parasite loses its home-field advantage. The future isn’t about eliminating risk, but about downgrading it from constant to controllable.
What You Can Do Today

Start with a conversation at your vet about year-round prevention that fits your household, including long-acting options if monthly dosing is hard to maintain. Put reminders on your phone, pair doses with a monthly bill, or keep the medication next to a routine task so it never gets skipped. Ask about annual testing for dogs and an individualized plan for cats, especially if coughing, lethargy, or breathing changes appear. For outdoor spaces, empty standing water, maintain screens, and time walks to avoid the mosquito rush at dawn and dusk.
Think beyond your own yard. Support local shelters and disaster-response programs that keep pets on prevention after storms, when risk skyrockets. If you move or adopt a pet from another region, test on arrival and maintain prevention without gaps. Small, steady steps across a community make the biggest dent in a disease that thrives on every missed chance.

Suhail Ahmed is a passionate digital professional and nature enthusiast with over 8 years of experience in content strategy, SEO, web development, and digital operations. Alongside his freelance journey, Suhail actively contributes to nature and wildlife platforms like Discover Wildlife, where he channels his curiosity for the planet into engaging, educational storytelling.
With a strong background in managing digital ecosystems — from ecommerce stores and WordPress websites to social media and automation — Suhail merges technical precision with creative insight. His content reflects a rare balance: SEO-friendly yet deeply human, data-informed yet emotionally resonant.
Driven by a love for discovery and storytelling, Suhail believes in using digital platforms to amplify causes that matter — especially those protecting Earth’s biodiversity and inspiring sustainable living. Whether he’s managing online projects or crafting wildlife content, his goal remains the same: to inform, inspire, and leave a positive digital footprint.




