Imagine a world where a tiny scrape on your knee could lead to a deadly infection, untreatable by any medicine we know. It sounds like something out of a post-apocalyptic movie, but this unsettling scenario is inching closer to reality each year. The culprit? Not some monstrous virus, but microscopic bacteria—ancient, clever, and shockingly social. These single-celled organisms have an unnerving trick up their sleeves: they can swap DNA like trading cards, passing along powerful survival tools, including resistance to the very antibiotics we depend on. The story of how they do this is as fascinating as it is frightening, revealing a hidden war raging just beneath the surface of our daily lives.
The Unseen World of Bacteria
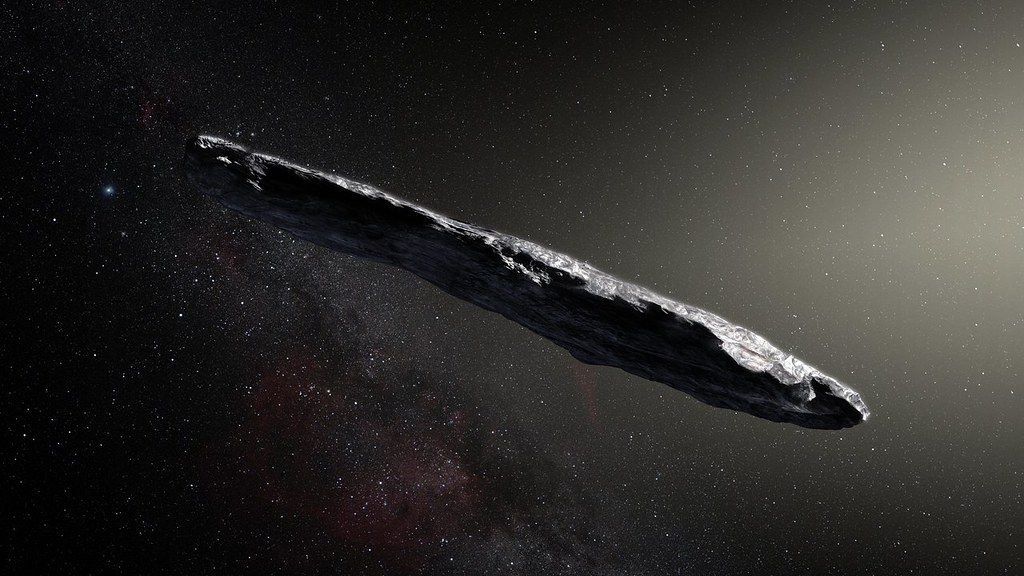
Bacteria are everywhere—on your skin, in your gut, on your doorknob. Most are harmless, and many are vital for life. But under a microscope, their true nature comes alive. They are tiny survival machines, thriving in boiling hot springs, icy glaciers, and even radioactive waste. Their adaptability is legendary, and much of it comes down to their ability to share genetic secrets with their neighbors. Think of bacteria as tiny, tireless inventors, always looking for the next big advantage. This inventiveness often puts them one step ahead of us.
What is DNA Sharing?
While humans inherit DNA only from their parents, bacteria can swap genetic material with almost any other bacterium they meet. This process, called horizontal gene transfer, lets bacteria quickly pick up new skills, such as antibiotic resistance. It’s like suddenly learning to play the piano just because your neighbor can. This DNA exchange isn’t rare—it happens all the time, right under our noses, quietly shaping the microbial world and, indirectly, our health.
Three Ways Bacteria Swap Genes
Bacteria have three main tricks for sharing DNA: transformation, transduction, and conjugation. Transformation is when bacteria pick up loose DNA from their environment, almost like scavenging scraps off the floor. Transduction happens when viruses infect bacteria, accidentally ferrying DNA from one bacterium to another. Conjugation, perhaps the most dramatic, involves a “bacterial handshake,” where two bacteria connect and pass genetic material directly. Each method is alarmingly efficient, helping bacteria outsmart threats in record time.
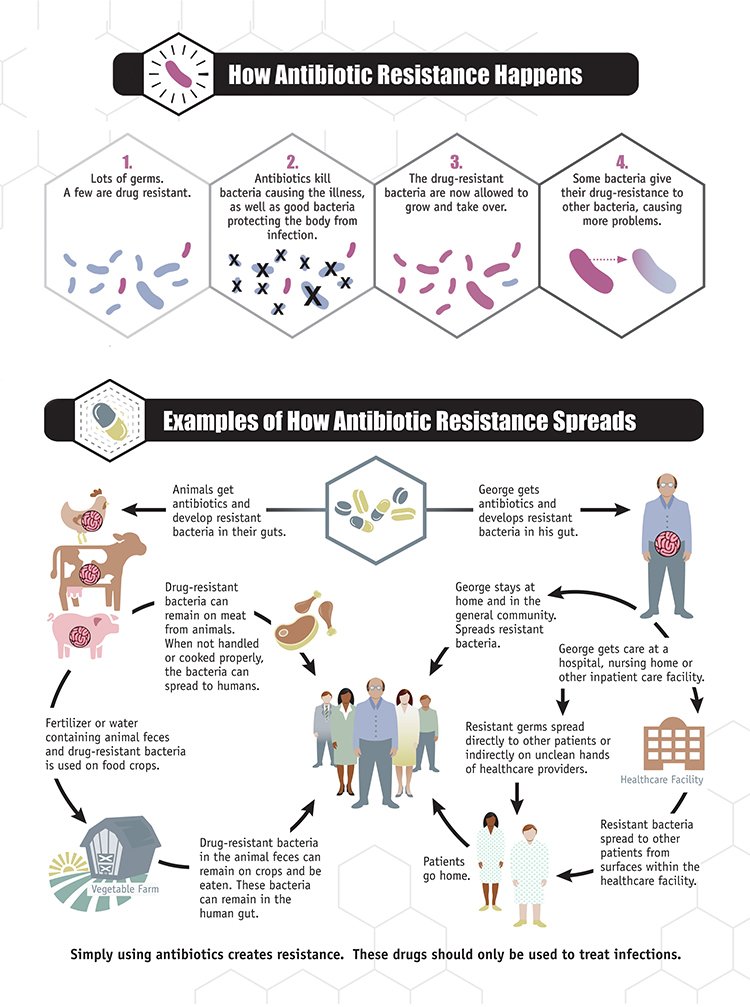
The Birth of Antibiotic Resistance
When antibiotics were first discovered, they were hailed as miracle drugs. But bacteria are fast learners. Through sharing DNA, they can quickly adapt, passing resistance genes between themselves like wildfire. One bacterium that survives a dose of antibiotics can teach countless others how to evade the drug, turning routine infections into potential nightmares. This is why some infections that were once easily treatable are now stubbornly resistant to even our strongest medicines.
Plasmids: The Genetic Messengers
A major player in bacterial DNA sharing is the plasmid—a small, circular piece of DNA separate from the main bacterial chromosome. Plasmids often carry genes for antibiotic resistance and can move between bacteria with shocking speed. Imagine if you could hand your friend a USB stick loaded with superpowers. That’s what plasmids do for bacteria, enabling them to spread resistance far and wide.
Hospitals: Hotspots for Resistance
Hospitals, meant to be places of healing, can ironically become breeding grounds for resistant bacteria. The heavy use of antibiotics in these environments puts intense pressure on bacteria to evolve. In crowded wards, bacteria mingle, swap genes, and multiply. This is why hospital-acquired infections are often the most difficult to treat—they’re the result of bacteria that have “seen it all” and learned to survive the harshest conditions.
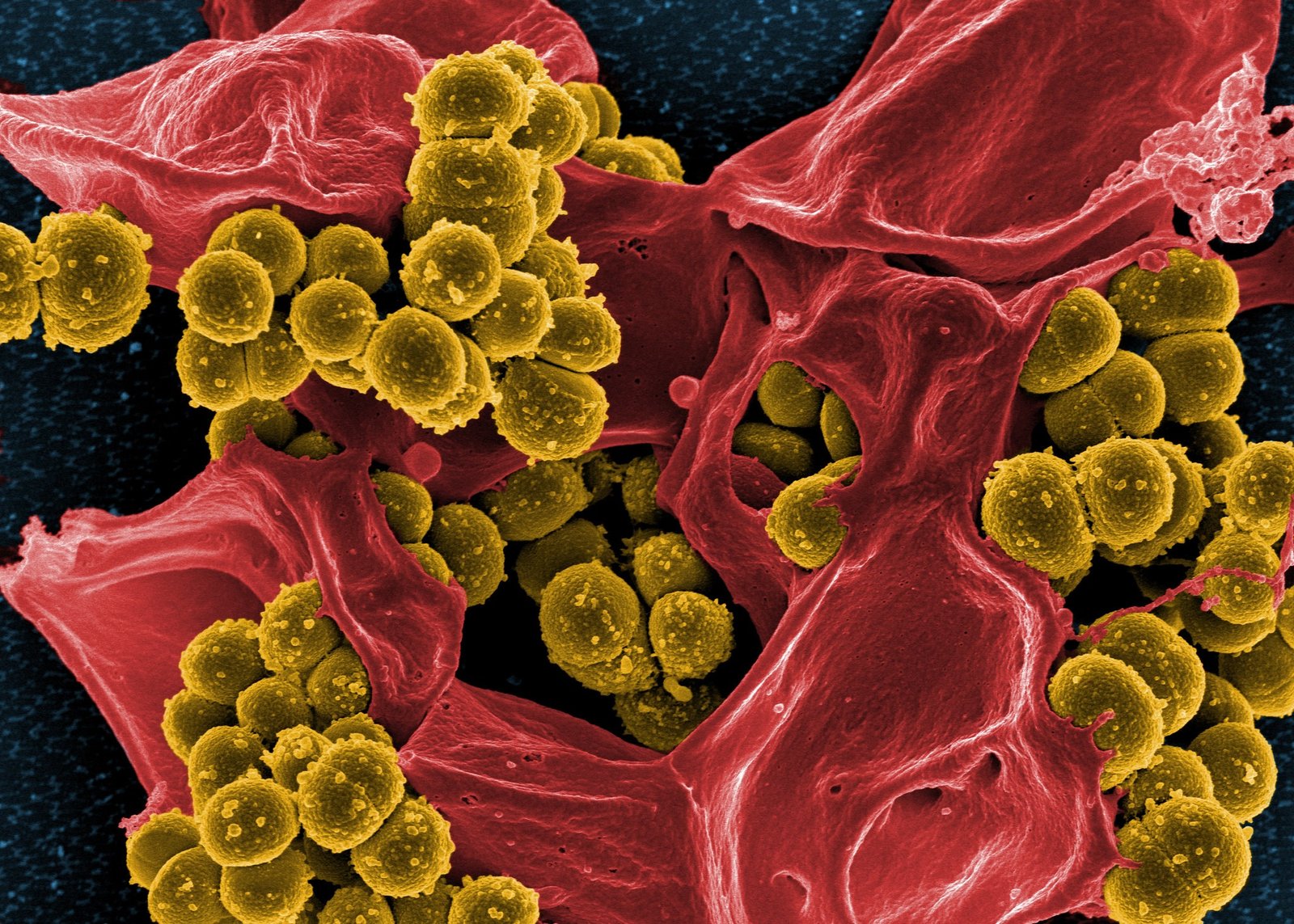
Superbugs: The Unseen Threat

Some bacteria have become so skilled at sharing resistance genes that they’re now known as “superbugs.” These are strains like MRSA and carbapenem-resistant Enterobacteriaceae, which can shrug off multiple antibiotics. Superbugs don’t care about hospital walls—they can travel on hands, doorknobs, and even through the air. In some cases, these infections are untreatable, turning minor illnesses into life-threatening situations.
Farming and Antibiotic Resistance
It’s not just hospitals where bacteria get creative. The use of antibiotics in agriculture—often to promote growth or prevent disease in livestock—provides another training ground for bacteria. Resistant bacteria can move from animals to humans through food, water, or direct contact. This creates a global web of resistance that doesn’t respect borders or species.
The Role of Wastewater and the Environment
When antibiotics and resistant bacteria end up in wastewater from hospitals, homes, and farms, they enter rivers, lakes, and soil. Bacteria in these environments meet and mingle, exchanging resistance genes in a microbial dance that knows no boundaries. This environmental spread means that even pristine natural areas are not immune to the march of resistance.
The Speed of Bacterial Evolution

Bacteria reproduce at lightning speed—sometimes doubling in number every 20 minutes. This rapid life cycle means that genetic changes, including resistance, spread incredibly fast. What takes humans thousands of years to evolve, bacteria can achieve in a matter of days or weeks. Their ability to share DNA supercharges this process, making them formidable opponents in the fight against disease.
Why Antibiotics Don’t Always Work

When bacteria become resistant, antibiotics that once worked stop having any effect. This can turn simple infections into chronic or even fatal conditions. Doctors are often forced to use older, more toxic drugs, or sometimes have no options left at all. The frustration is palpable—imagine using every tool in your toolbox, only to find nothing works.
The Global Crisis of Resistance
Antibiotic resistance isn’t just a local problem—it’s a global crisis. Resistant bacteria travel with people, animals, and goods, crossing continents with ease. The World Health Organization has called this one of the biggest threats to global health today. Without urgent action, we risk returning to a time when even minor injuries or routine surgeries could be deadly.
The Human Cost of Resistance
Behind the statistics are real people—children, grandparents, friends—whose lives are cut short by infections that should have been easily cured. Families watch loved ones suffer as doctors run out of options. The emotional toll is immense, and the fear of untreatable infections is growing. It’s a stark reminder that scientific progress can be undone if we’re not careful.
New Weapons in the Fight
Scientists are racing to find new antibiotics, but the pipeline is drying up. It’s a bit like patching a leaking boat while the water keeps rising. Innovative approaches—like phage therapy, which uses viruses to attack bacteria, or harnessing the immune system—offer hope. Still, the best defense is slowing the spread of resistance in the first place.
Prevention: The Power is in Our Hands
Everyone can play a part in fighting antibiotic resistance. Simple steps, like only using antibiotics when necessary, finishing prescribed courses, and practicing good hygiene, can make a huge difference. Healthcare workers are learning to prescribe more carefully, and farmers are seeking alternatives to routine antibiotic use. Small changes, multiplied across millions of people, can slow the spread of resistance.
The Importance of Research and Surveillance
Tracking resistance is like keeping an eye on a wildfire—knowing where it’s spreading helps us respond faster. Scientists study patterns of resistance in hospitals, communities, and the environment, looking for hotspots and new threats. This research informs policies and helps target interventions where they’re needed most.
Education: Spreading Awareness
Many people don’t realize how serious antibiotic resistance is until it affects them personally. Education campaigns are crucial—teaching the public, healthcare workers, and even children about the dangers of overusing antibiotics. The more people understand, the more likely they are to take precautions and demand action from leaders.
The Role of Vaccines
Vaccines can help reduce the need for antibiotics by preventing bacterial infections in the first place. By keeping people healthy, vaccines reduce the opportunities for bacteria to develop resistance. This is especially important for vulnerable groups, like young children and the elderly, who are most at risk from resistant infections.
An Unfinished Battle
The fight against antibiotic resistance is far from over. Bacteria have been evolving for billions of years, and they won’t stop now. But human creativity, determination, and cooperation offer hope. By understanding how bacteria share DNA and spread resistance, we can all play a role in protecting the medicines that have saved so many lives. Are you ready to join the fight?