Imagine if your body’s greatest defender suddenly turned against you, launching an attack so fierce it became more dangerous than the original threat. That’s the unsettling reality of a cytokine storm—a phenomenon that can transform the immune system from a vigilant guardian into a reckless foe. For many, the term first burst into the spotlight during the COVID-19 pandemic, but its story is much older, woven through the annals of medicine and human survival. This hidden tempest inside the body is at once fascinating and frightening, a reminder that nature’s most powerful forces often lie within ourselves. Let’s venture together into the world of cytokine storms—where biology, mystery, and drama collide.
The Immune System: Nature’s Bodyguard
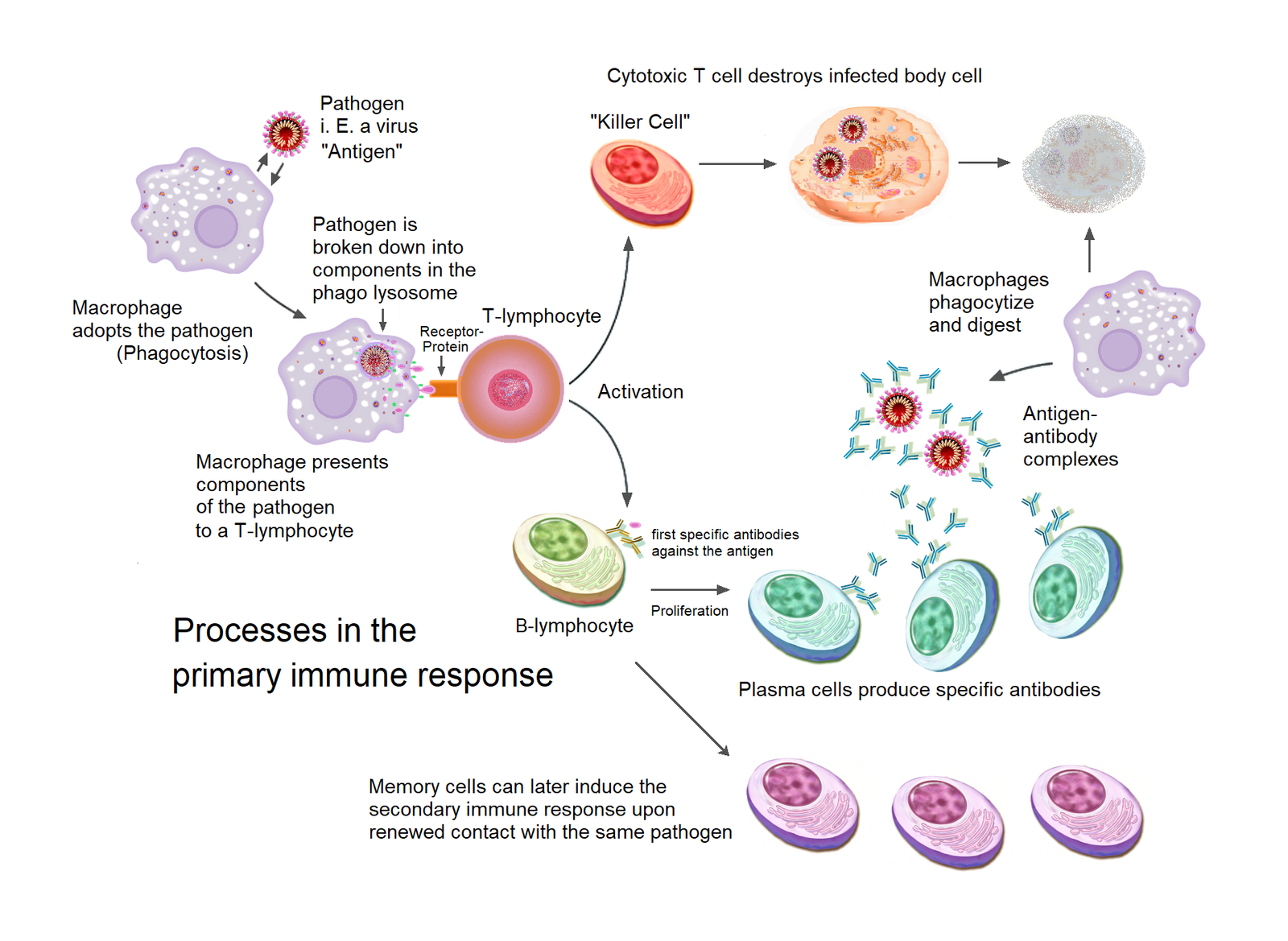
Our immune system is like a silent, loyal bodyguard, always patrolling for invaders. It’s made up of specialized cells, proteins, and organs working together in harmony. When viruses or bacteria sneak in, immune cells like T-cells and macrophages leap into action, releasing chemical messengers called cytokines. Cytokines help coordinate the attack, calling in reinforcements and ramping up defenses. Think of them as text messages sent between immune cells, ensuring everyone knows what to do. This complex dance usually keeps us healthy, stopping threats before we even notice. But sometimes, the messages get garbled or overblown—and that’s where trouble starts.
Cytokines: The Immune System’s Tiny Messengers
Cytokines are small proteins, but don’t let their size fool you—they wield enormous power. They act as the directors of the immune response, telling cells when to multiply, move, or even self-destruct. There are many types, including interleukins, interferons, and tumor necrosis factors. Each has its own job, like a conductor leading a symphony. When the right balance is struck, the immune system hums beautifully. But if cytokines are released in excess, chaos can erupt within the body. This delicate balance is crucial for survival, and even a slight misstep can have dramatic effects.
What Exactly Is a Cytokine Storm?
A cytokine storm is an extreme immune reaction where the body releases far too many cytokines in a short time. Instead of a precise strike, the immune system unleashes a tidal wave of chemicals that can overwhelm tissues and organs. It’s like sounding every alarm at once—what starts as a targeted defense becomes a wildfire raging out of control. Blood vessels can leak, blood pressure may plummet, and organs struggle to function. The storm can be more deadly than the infection itself, turning the immune system’s power against its own host.
The First Clues: Early Signs and Symptoms
Recognizing a cytokine storm isn’t always straightforward, but certain warning signs stand out. Symptoms often include high fever, severe fatigue, muscle pain, and difficulty breathing. As the storm intensifies, patients may develop dangerously low blood pressure, confusion, or even multi-organ failure. The experience can be terrifying—one moment, someone may have a routine infection, the next, their body is in crisis. Medical teams look for rapid changes in vital signs, lab tests showing high inflammation, and clinical features that don’t match typical infections.
Why Does the Immune System Go Rogue?

It’s a question that baffles even seasoned scientists: why would a body attack itself so fiercely? Sometimes, a particularly aggressive virus or bacteria tricks the immune system into overreacting. Other times, genetic differences or underlying health problems make some people more vulnerable to runaway inflammation. Infections like influenza, SARS, and more recently COVID-19 have all been linked to cytokine storms. The exact reasons are complex and still under investigation, but it’s clear that both nature and nurture play a part.
Famous Outbreaks and Historical Cases
The world first witnessed the devastating power of cytokine storms during the 1918 Spanish flu pandemic. Many young, healthy adults suddenly succumbed not to the virus, but to their own immune systems’ overzealous response. Decades later, SARS, avian flu, and Ebola outbreaks showed similar patterns. Most recently, during the COVID-19 crisis, doctors observed severe cases where cytokine storms led to rapid deterioration. Each event has taught researchers more about the phenomenon, yet its unpredictability remains a challenge.
The Science Behind the Storm: What Goes Wrong?
Underneath the symptoms lies a tangled web of molecular confusion. In a cytokine storm, molecules like IL-6, TNF-alpha, and interferons surge in the bloodstream. These chemicals make blood vessels leaky, attract more immune cells, and ramp up inflammation everywhere. The body’s tissues—lungs, heart, liver, kidneys—can swell and become damaged as a result. Imagine a neighborhood fire alarm system going off in every house, even those without a fire. The chaos can quickly spiral, making recovery difficult.
Cytokine Storms in COVID-19: Lessons Learned
The COVID-19 pandemic cast a harsh spotlight on cytokine storms, especially in patients with severe pneumonia. Doctors noticed that some people’s lungs filled with fluid, their oxygen levels dropped, and their bodies shut down despite aggressive treatment. Blood tests often revealed sky-high levels of inflammatory markers. This led to a global scramble for answers, with researchers racing to find ways to calm the immune system without leaving patients defenseless. The crisis underscored the importance of understanding cytokine regulation in modern medicine.
How Do Doctors Diagnose a Cytokine Storm?
Diagnosing a cytokine storm is a bit like solving a mystery, requiring sharp clinical skills and advanced laboratory tools. Doctors look for clusters of symptoms, sudden worsening, and evidence of systemic inflammation. Blood tests measuring ferritin, C-reactive protein, and specific cytokines give important clues. Imaging scans may show organ swelling or fluid buildup. Ultimately, diagnosis is part art, part science—a careful weighing of evidence to distinguish a storm from a typical infection.
Who’s at Risk? The Vulnerable and the Unlucky
Not everyone exposed to a dangerous pathogen develops a cytokine storm. Certain groups are at higher risk: people with autoimmune diseases, the elderly, those with chronic illnesses, and even some seemingly healthy young adults. Genetics may play a role—some individuals’ immune systems are simply more prone to overreacting. Environmental factors, stress, and underlying health can also tip the balance. It’s a sobering reminder that biology doesn’t always play fair.
The Role of Genetics: Are Some People Predisposed?
Recent research suggests that our DNA can influence how likely we are to experience a cytokine storm. Specific genetic mutations may make some immune systems more reactive or less able to shut down inflammation once it starts. Family history sometimes offers clues, with clusters of severe reactions occurring in certain lineages. Scientists continue to hunt for these genetic markers, hoping that one day we can predict or even prevent these dangerous storms.
Beyond Viruses: Other Triggers of Cytokine Storms
While infections are the most common culprits, cytokine storms can be triggered by other causes too. Certain cancers, autoimmune diseases, and reactions to some medical treatments—like CAR T-cell therapy for leukemia—have all been linked to runaway cytokine release. Even some medications and environmental toxins might spark a storm in rare cases. This wide range of triggers makes the phenomenon especially tricky for doctors to anticipate and manage.
Treatment Strategies: Calming the Storm
Managing a cytokine storm is a medical tightrope walk. The goal is to dampen the harmful inflammation without shutting down the body’s ability to fight the original threat. Steroids like dexamethasone, biologic drugs that block specific cytokines, and supportive care like oxygen and fluids are often used. Doctors may also employ therapies such as plasmapheresis, which filters inflammatory molecules from the blood. Each case requires a personalized approach, and timing is critical—too early or too late can mean the difference between recovery and tragedy.
Groundbreaking Research and Emerging Therapies
Scientists are racing to find better ways to predict, detect, and treat cytokine storms. New drugs targeting specific cytokines are in development, aiming to neutralize the storm without compromising other immune functions. Researchers are also exploring gene therapies, novel biomarkers, and advanced artificial intelligence tools to help spot storms before they escalate. The field is moving fast, driven by the urgency of recent pandemics and the promise of saving more lives.
Living Through a Cytokine Storm: Patient Stories
For those who survive a cytokine storm, the experience is often life-changing. Patients describe feeling like they were drowning from within, their bodies betraying them in the fight for survival. Many spend days or weeks in intensive care, facing uncertainty and fear. Family members, too, are swept up in the turmoil, waiting anxiously for signs of improvement. Recovery can be slow, with lingering fatigue and emotional scars—a testament to the storm’s ferocity.
The Global Impact: What Cytokine Storms Teach Us
Cytokine storms have reshaped the way doctors think about infections and immunity. They highlight the need for rapid response, better diagnostics, and smarter treatments. Countries and health organizations now include cytokine storm management in pandemic preparedness plans. The phenomenon also sparks broader debates about the balance between fighting disease and protecting the body from its own defenses. Each new outbreak brings hard lessons—and hope for new solutions.
Preventing the Next Storm: What Can We Do?
While it’s impossible to eliminate the risk of cytokine storms entirely, there are steps individuals and communities can take. Staying up-to-date on vaccinations, managing chronic illnesses, and seeking prompt care for severe infections are all crucial. On a larger scale, investing in medical research, strengthening healthcare systems, and promoting public health awareness help prepare societies for future challenges. Everyone plays a part, from scientists at the bench to patients in the clinic.
Hope on the Horizon: The Future of Immunology
The study of cytokine storms has opened up new frontiers in immunology, inspiring scientists to rethink old ideas. Advances in genetic testing, personalized medicine, and drug development promise better outcomes in the years to come. The ultimate goal is to harness the immune system’s power without letting it run amok—a dream that’s slowly coming into sharper focus. The journey is far from over, but every discovery brings us closer to understanding and controlling the storm within.
Reflections: The Immune System’s Double-Edged Sword
Cytokine storms remind us that our bodies are both fragile and resilient, capable of astonishing feats and unexpected betrayals. The same forces that protect us can, under rare circumstances, become our greatest threat. This paradox lies at the heart of human biology—a thrilling, sometimes terrifying balancing act that shapes the course of life itself. As we learn more about cytokine storms, one truth stands out: the line between friend and foe is often thinner than we think.




