Life moves fast these days, and stress seems to lurk around every corner. But what happens when that tension we carry goes deeper than we realize? Recent research reveals something that might shock you – stress doesn’t just make us feel overwhelmed. It literally rewrites our bodies at the most fundamental level, altering our cells in ways that can affect our health for years to come. The discoveries scientists are making about stress and cellular changes paint a picture that’s both alarming and fascinating. Chronic stress has been shown to shorten telomeres, the protective caps on our DNA, essentially speeding up the clock on cellular aging. Stress hormones like cortisol flood the system, disrupting normal immune responses and leaving us more vulnerable to illness. Even the mitochondria—the tiny powerhouses inside our cells—struggle under prolonged strain, reducing our body’s energy supply. Over time, these invisible changes can manifest as heart disease, diabetes, and even cognitive decline. It’s a reminder that stress isn’t just in our heads—it’s etched into our biology, shaping our future health one cell at a time.
The Silent Transformation Your Body Undergoes During Stress

When stress hits, your body triggers what’s called the fight-or-flight response, but this ancient survival mechanism wasn’t designed for modern life. The rush of adrenaline and noradrenaline secreted from the adrenal medulla leads to a widespread discharge of almost all portions of the sympathetic system throughout the body, with increased secretion of norepinephrine and epinephrine from the adrenal medulla into the circulation. The immediate effects are noticeable – your heart pounds, your breathing changes, and you feel energized.
However, what you can’t feel is even more significant. When released, norepinephrine and epinephrine bind to specific membrane-bound G-protein receptors to initiate an intracellular cyclic adenosine monophosphate (cAMP) signaling pathway that rapidly activates cellular responses. This means stress hormones directly communicate with your cells, changing how they function at their most basic level. The transformation begins within minutes, setting off a cascade of molecular events that can persist long after the stressful situation ends.
How Stress Hijacks Your Cellular Energy Factories
Your cells depend on tiny powerhouses called mitochondria to produce the energy they need to function. But chronic stress can literally damage these critical structures. The fight-or-flight response can often lead to mitochondrial damage in bodies, where the mitochondria’s main function is to provide energy for the rest of the body through cellular respiration. Think of it like forcing your car engine to constantly run at maximum RPM – eventually, something’s going to break.
When mitochondria become damaged, cells struggle to produce adequate energy. Since stress often results in these physical symptoms, the body needs to put more pressure on the mitochondria to make more energy. This creates a vicious cycle where stressed cells need more energy but have compromised ability to produce it. The result? Cells begin to dysfunction, and you might experience fatigue, brain fog, or other symptoms that seem to have no obvious cause.
The DNA Damage Response That Never Stops
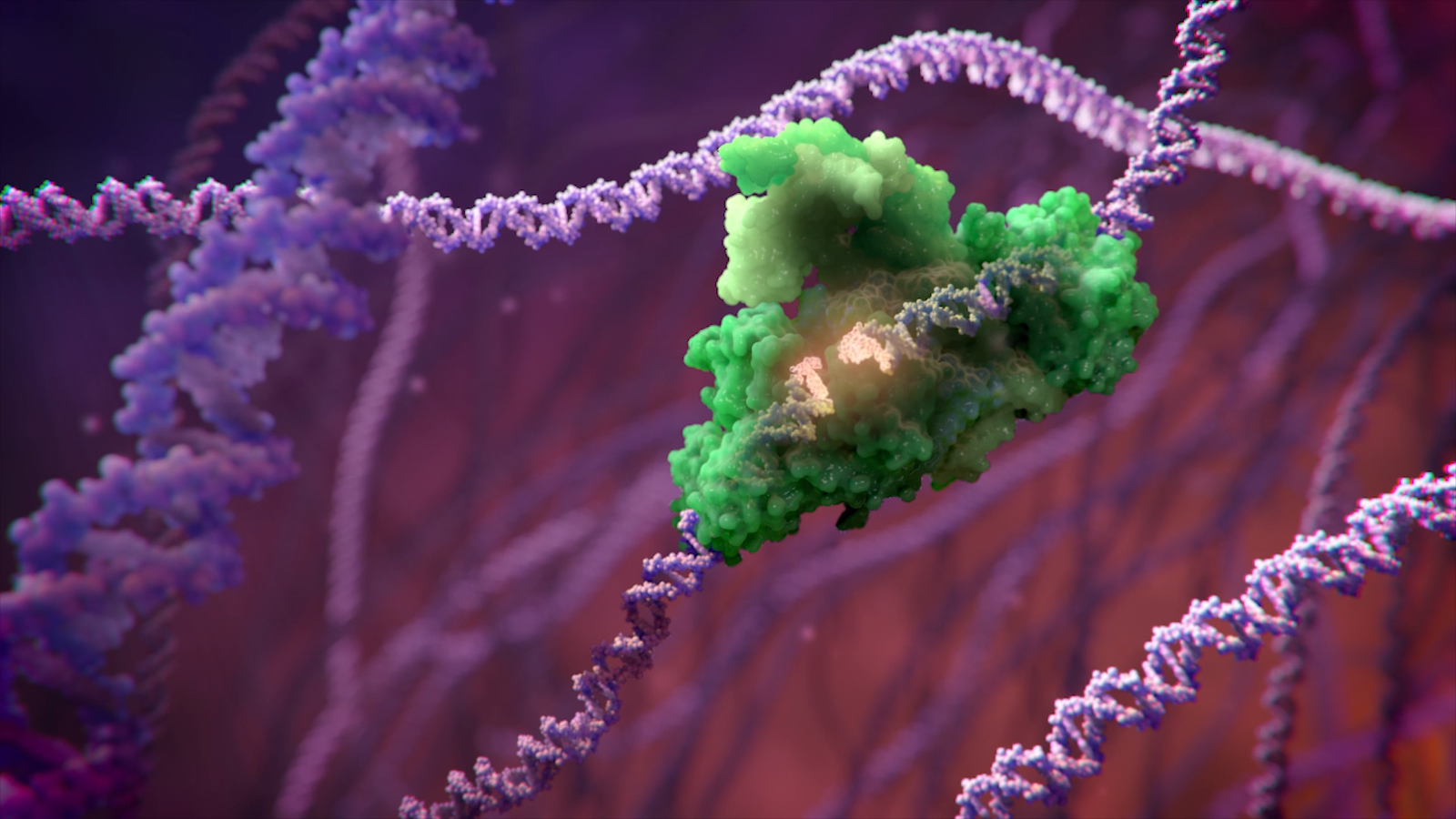
Cellular stress can be broadly defined as disturbances of the internal environment ranging from a shift in usual (homeostatic) cellular conditions to severe assaults that damage the structure or functions within cells, and cellular stress responses exist to detect the effects of stress on cells. When cells detect damage, they activate protective mechanisms. But here’s where things get complicated – sometimes these protective responses never turn off.
Cells can respond to stress in various ways ranging from the activation of survival pathways to the initiation of cell death that eventually eliminates damaged cells, and depending on the level and mode of stress, different defense mechanisms and prosurvival strategies are mounted. Picture a city where the emergency sirens never stop blaring. Eventually, the constant state of alert becomes more harmful than helpful, leading to cellular dysfunction and premature aging.
Oxidative Stress: When Your Cells Rust From the Inside

One of the most damaging effects of chronic stress involves oxidative damage. Oxidative stress is when an excess of molecules called free radicals in your body start to cause damage, and anything that raises the number of free radicals in your body to unhealthy levels can cause oxidative stress. These free radicals are like molecular rust, corroding your cellular machinery from within.
Extensive sun exposure, stress and smoking can cause your body to make more free radicals than it needs. Your body normally produces antioxidants to neutralize these harmful molecules, but chronic stress overwhelms these natural defenses. You might not always know your body is experiencing oxidative stress as it involves tiny, microscopic changes that go on behind the scenes. The damage accumulates silently, contributing to premature aging and disease development.
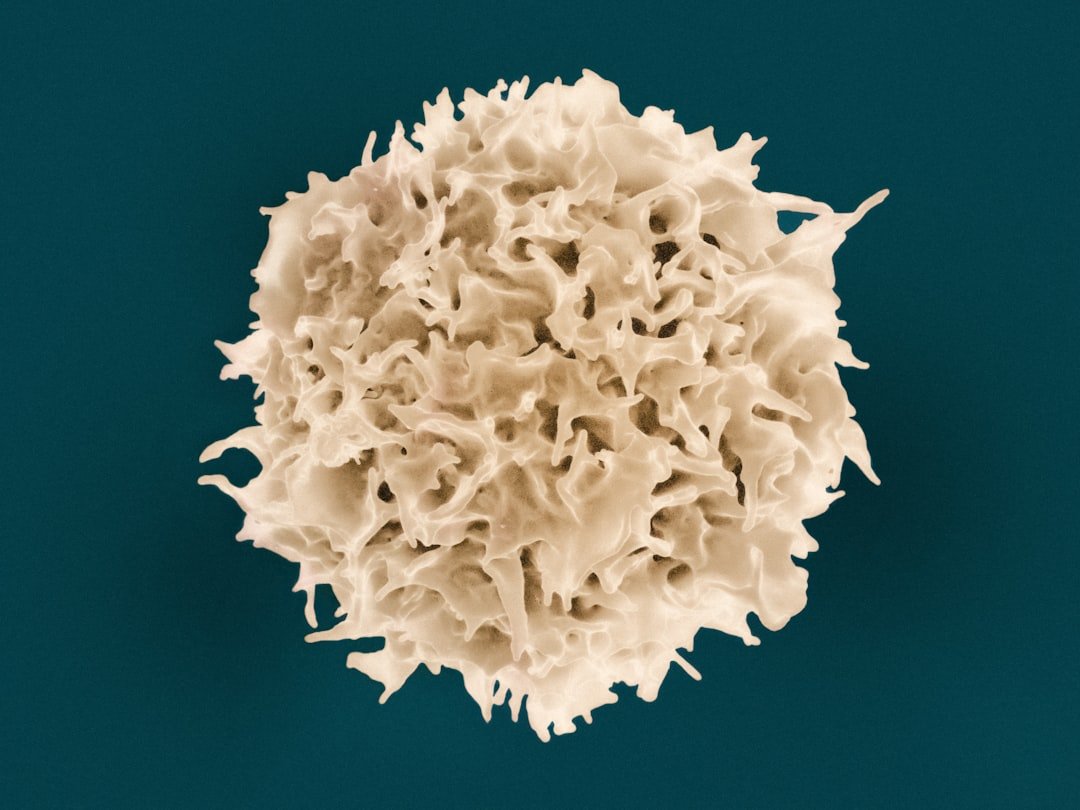
Telomeres: The Cellular Clocks That Stress Speeds Up
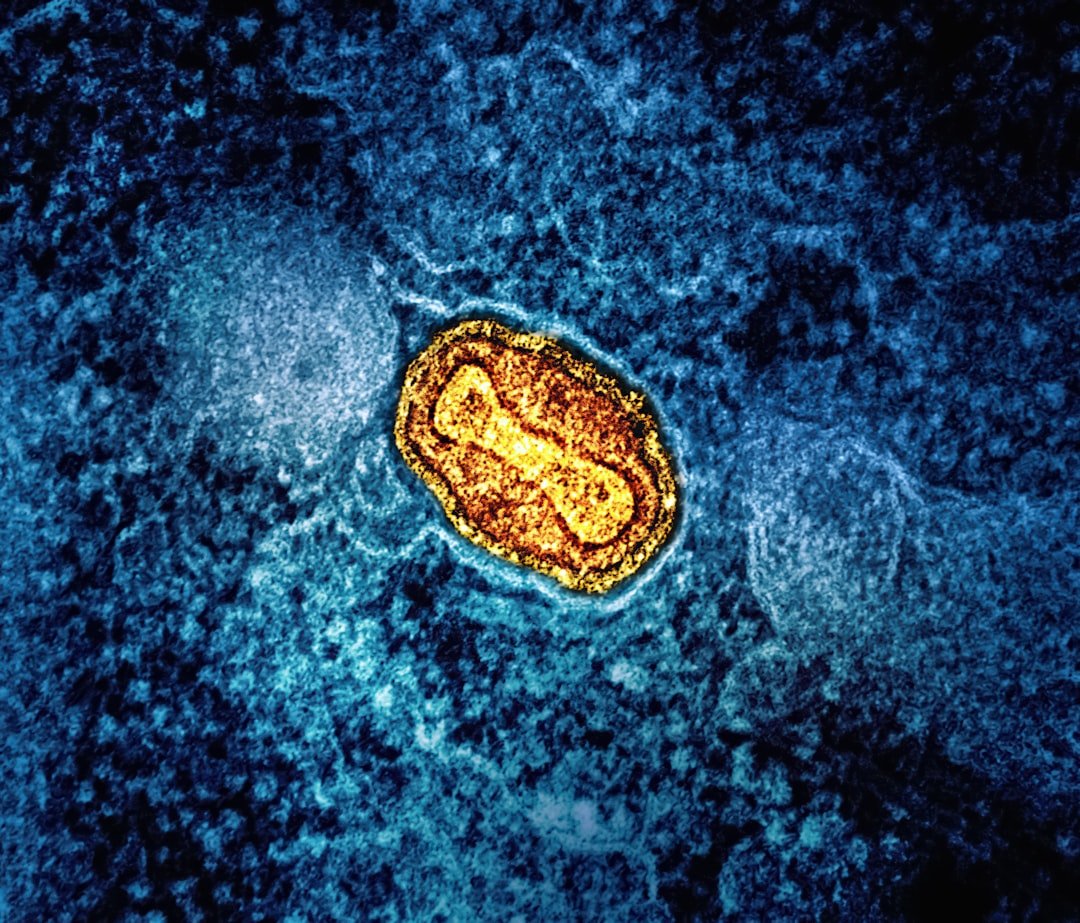
At the tips of your chromosomes lie protective structures called telomeres, which scientists often compare to the plastic caps on shoelaces. Telomeres protect our genetic data, make it possible for cells to divide, and hold some secrets to how we age and get cancer, as they have been compared with the plastic tips on shoelaces, because they keep chromosome ends from fraying and sticking to each other. Each time a cell divides, these telomeres get shorter.
Here’s where stress becomes particularly insidious: These findings have implications for understanding how, at the cellular level, stress may promote earlier onset of age-related diseases, as numerous studies demonstrate links between chronic stress and indices of poor health. Research shows that people under chronic stress have significantly shorter telomeres than their less-stressed counterparts. Oxidative stress can induce DNA damage and may therefore expedite telomere shortening. It’s as if stress makes your cellular clocks tick faster, accelerating the aging process at the molecular level.
The Inflammatory Fire That Stress Ignites
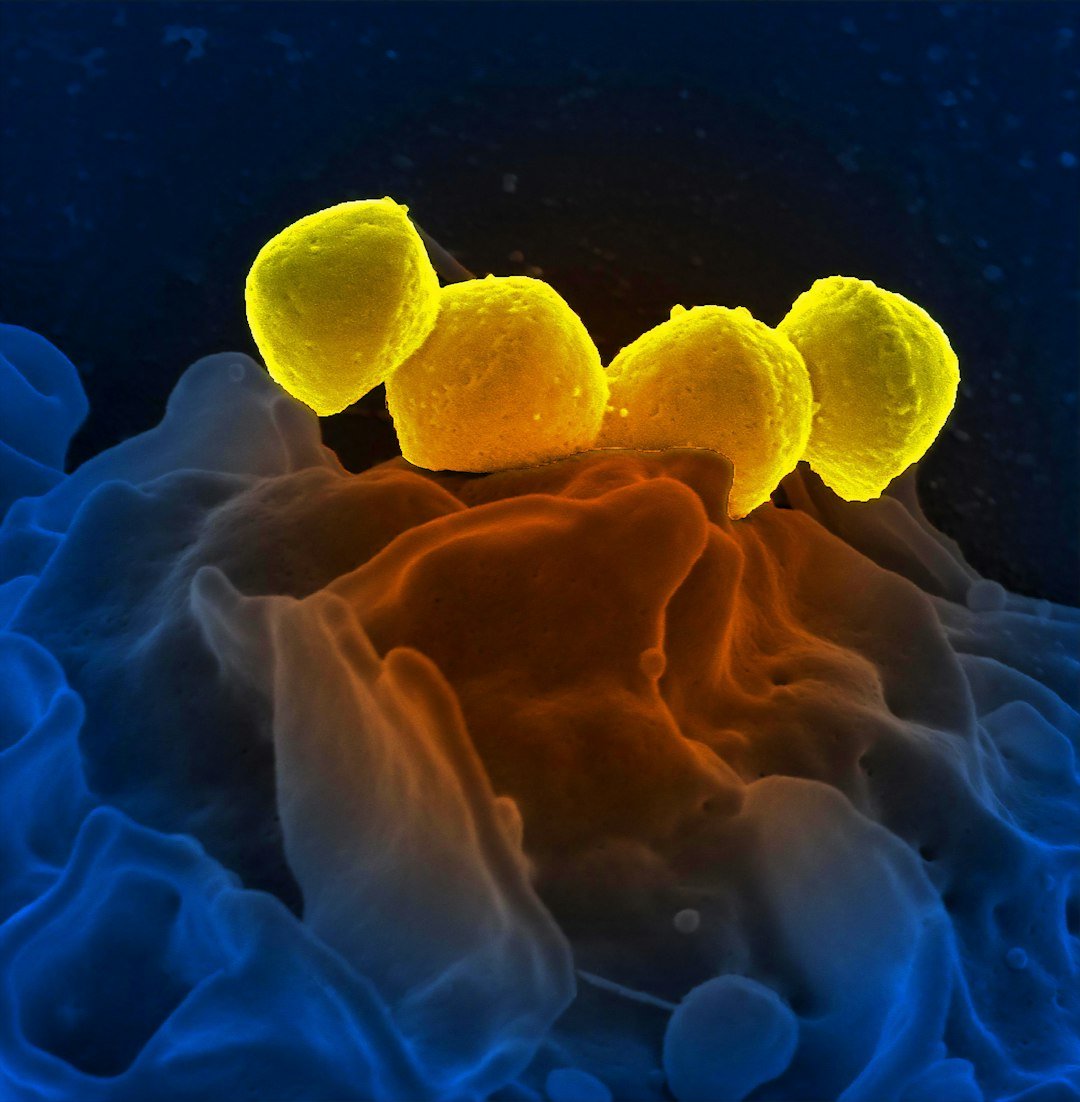
Chronic stress triggers a complex inflammatory response throughout your body. The cells that make up your immune system, or immune cells, release most of your body’s cytokines, which are proteins that help control inflammation in your body. These cytokines are like chemical messengers that coordinate your immune response, but chronic stress can cause them to go haywire.
The presence of these stress hormones promotes oxidative stress, endothelial dysfunction, and inflammation, thereby promoting the development of atherosclerosis and compromising vascular function. When inflammation becomes chronic, it stops being helpful and starts being destructive. Too many cytokines can create a heightened inflammatory response, and too much inflammation can damage tissue and lead to diseases and conditions. Your body essentially begins attacking itself, mistaking healthy tissue for threats.
How Stress Rewrites Your Immune Cell Programming
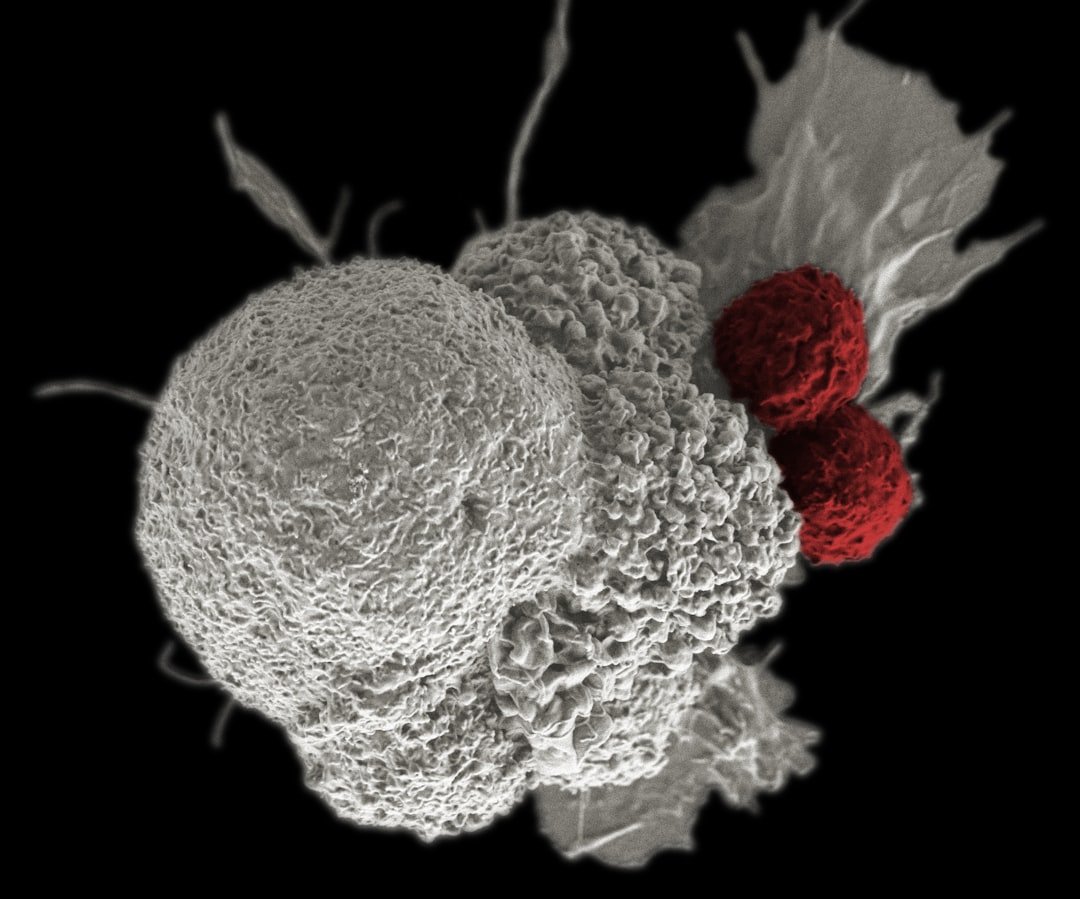
The immune system under chronic stress undergoes dramatic changes that can persist long after the stressor is removed. Chronic stress leads to various diseases, mainly through the activation of hypothalamus-pituitary-adrenal (HPA) axis and sympathetic nervous system (SNS) axis, while chronic stress inhibits proinflammatory cytokines secretion which mediate the cellular immunity. This creates an imbalanced immune response.
Th1 cells primarily secrete IL-2, IL-6, TNF-α, and INF-γ, which activate cytotoxic T cells, natural killer cells, and macrophage, whereas Th2 cells secrete a different set of cytokines, primarily IL-4, IL-10, and IL-13, which promote humoral immunity. Chronic stress shifts the balance between these immune responses, potentially making you more susceptible to infections and slower to heal from injuries. Your immune cells literally change their behavior patterns, like switching from offensive to defensive players in the middle of a game.
The Cellular Memory of Trauma and Chronic Stress
Perhaps most disturbing is the discovery that stress can create lasting changes in cellular function. Stress is known to activate distinct neuronal circuits in the brain and induce multiple changes on the cellular level, including alterations in neuronal structures. These changes don’t just affect brain cells – they ripple throughout the entire body.
These dynamic cellular processes are accelerated during stress when neurotransmitter concentrations are elevated, and various experiments have shown that during stress, noradrenergic and adrenergic neurons release more noradrenaline and adrenaline. The cellular machinery that normally maintains balance becomes overactive and eventually dysregulated. It’s like having a thermostat that gets stuck – the system keeps trying to respond to signals that are no longer accurate.
When Cells Choose Death Over Dysfunction
Sometimes, the cellular damage from chronic stress becomes so severe that cells make the ultimate sacrifice. The mechanism by which a cell dies, that is, apoptosis, necrosis, pyroptosis, or autophagic cell death, often depends on its ability to cope with the conditions to which it is exposed, and activation of death signaling pathways is the ultimate response to all types of persistent irresolvable stress.
While programmed cell death might sound alarming, it’s actually a protective mechanism. In most circumstances, the induction of an autophagic response serves as a strategy that should ensure the cell’s survival. However, when too many cells in vital organs begin dying off due to chronic stress, it contributes to tissue deterioration and organ dysfunction. This cellular sacrifice helps explain why chronic stress is linked to so many different health problems – from heart disease to immune disorders.
The Adaptive Response That Becomes Maladaptive
Recent groundbreaking research has revealed that cells don’t respond to stress in the rigid, one-size-fits-all manner scientists once believed. Researchers at Case Western Reserve University have discovered a cell’s response is more nuanced and compartmentalized – not fixed or rigid, as previously thought, suggesting this adaptive response to stress could potentially be exploited to kill cancer cells.
ISR is not a one-size-fits-all system like we used to think. Instead, it can change and adjust depending on the type, strength and length of the stress the cell is experiencing. This discovery opens new possibilities for understanding why some people seem more resilient to stress than others. However, it also reveals that prolonged stress can cause these adaptive systems to become maladaptive, where the very mechanisms designed to protect cells begin to harm them instead.
Breaking the Cycle: What This Means for Your Health

Understanding how stress affects us at the cellular level isn’t just academic – it has profound implications for health and healing. In recent years, telomeres have emerged not only as biomarkers, but as mediators through which chronic psychosocial stress leads to diseases, and over the last seventeen years, a growing literature links stress to alterations in telomerase activity and telomere shortening.
The good news is that many of these cellular changes aren’t necessarily permanent. The rate of telomere shortening can be either increased or decreased by specific lifestyle factors, and better choice of diet and activities has great potential to reduce the rate of telomere shortening or at least prevent excessive telomere attrition. Your cells have remarkable capacity for repair and regeneration when given the right conditions. The key is recognizing that stress management isn’t just about feeling better – it’s about protecting your cellular health and potentially adding years to your life.
Conclusion

The science of stress and cellular health reveals a truth that’s both sobering and empowering. While chronic stress can literally rewrite our bodies at the molecular level – damaging mitochondria, shortening telomeres, triggering inflammation, and disrupting immune function – our cells also possess incredible resilience. Understanding these mechanisms helps explain why stress management isn’t a luxury but a biological necessity.
The next time you feel overwhelmed, remember that the stakes are higher than just emotional well-being. Your cells are listening, responding, and adapting to every stressful moment. But they’re also capable of healing, regenerating, and thriving when you give them what they need. Isn’t it amazing how something as simple as managing stress could be one of the most powerful things you can do for your cellular health?




