Imagine waking up one morning struggling for breath, a dull ache deep in your chest, and a relentless cough that refuses to fade. Now, picture learning that the true culprit is not a virus or bacteria, but a silent invader—an invisible fungus quietly feasting on your lungs from within. This isn’t science fiction. Under the right conditions, a group of fungi known as Aspergillus can turn your lungs into their personal buffet, making this bizarre and terrifying scenario a reality for thousands each year.
The Invisible Enemy: What Is Aspergillus?
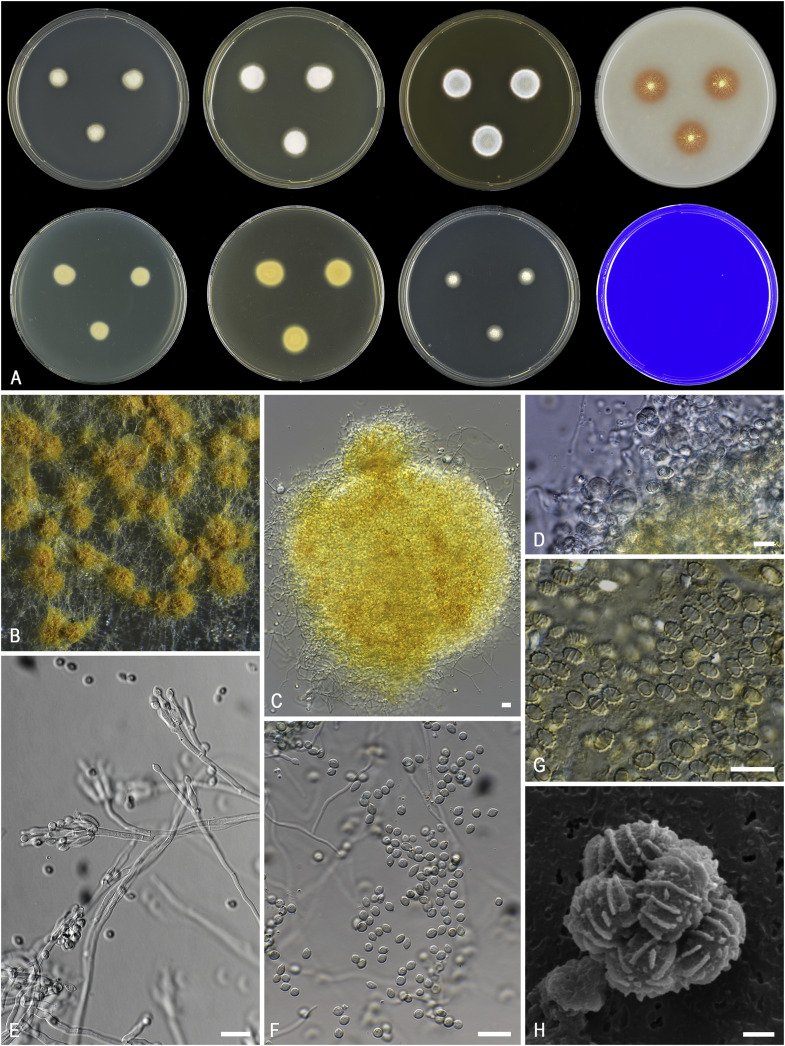
Aspergillus is a common mold found in soil, decaying leaves, and even household dust. Most people breathe in its spores daily without a second thought or any sign of illness. But for some, these spores can become a nightmare. Aspergillus is particularly dangerous because it is resilient and adaptable, thriving in environments where many other microorganisms would perish. In healthy people, the immune system quickly clears out these invaders. However, when the immune system is weakened, Aspergillus can take hold, settling deep into the moist, warm recesses of the lungs. Here, it begins its silent assault, surviving off the very tissues meant to keep us alive.
How Does a Fungus Invade the Lungs?
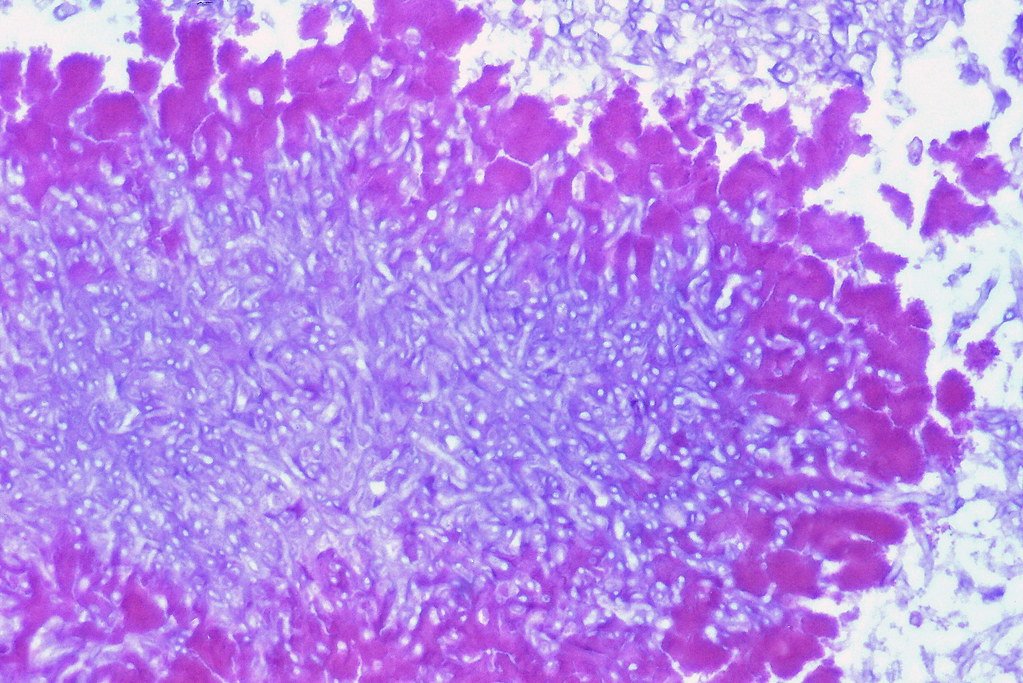
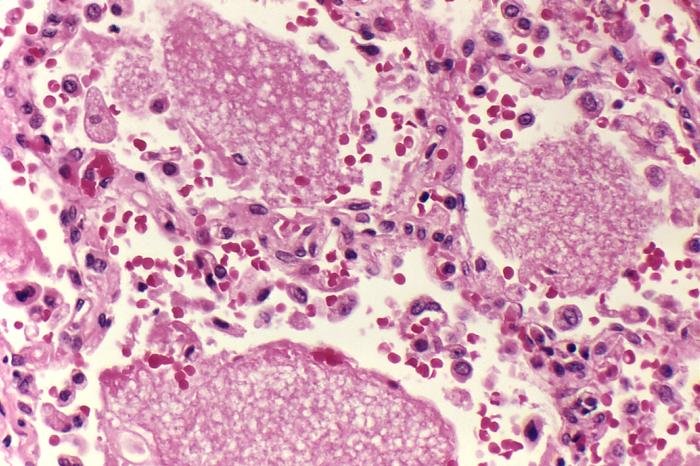
The process starts with spores—microscopic, dust-like seeds drifting through the air. When inhaled, these spores can lodge themselves within the tiny airways of the lungs. In most healthy individuals, the immune system acts like a vigilant guard, identifying and destroying these foreign particles before they can do harm. But in those with compromised immunity—such as cancer patients, organ transplant recipients, or people with chronic lung diseases—these spores find an open door. They germinate, spreading fine threads called hyphae that burrow through lung tissue. This is how Aspergillus begins to eat away at the lungs from the inside out, causing damage that is both shocking and difficult to reverse.
Who Is Most at Risk?
Not everyone who breathes in Aspergillus spores will become ill. The fungus is opportunistic, waiting for the perfect storm of vulnerability to strike. People with weakened immune systems are most at risk—think of those undergoing chemotherapy, individuals living with HIV/AIDS, or patients on long-term steroids. Chronic lung conditions like asthma, cystic fibrosis, or tuberculosis scars can also create pockets where the fungus can settle and multiply. Even construction workers and farmers, frequently exposed to dust and decaying plant material, may find themselves more susceptible if their defenses are down. For these individuals, what is usually a harmless breath of air can become a life-threatening exposure.
Signs and Symptoms: When to Worry
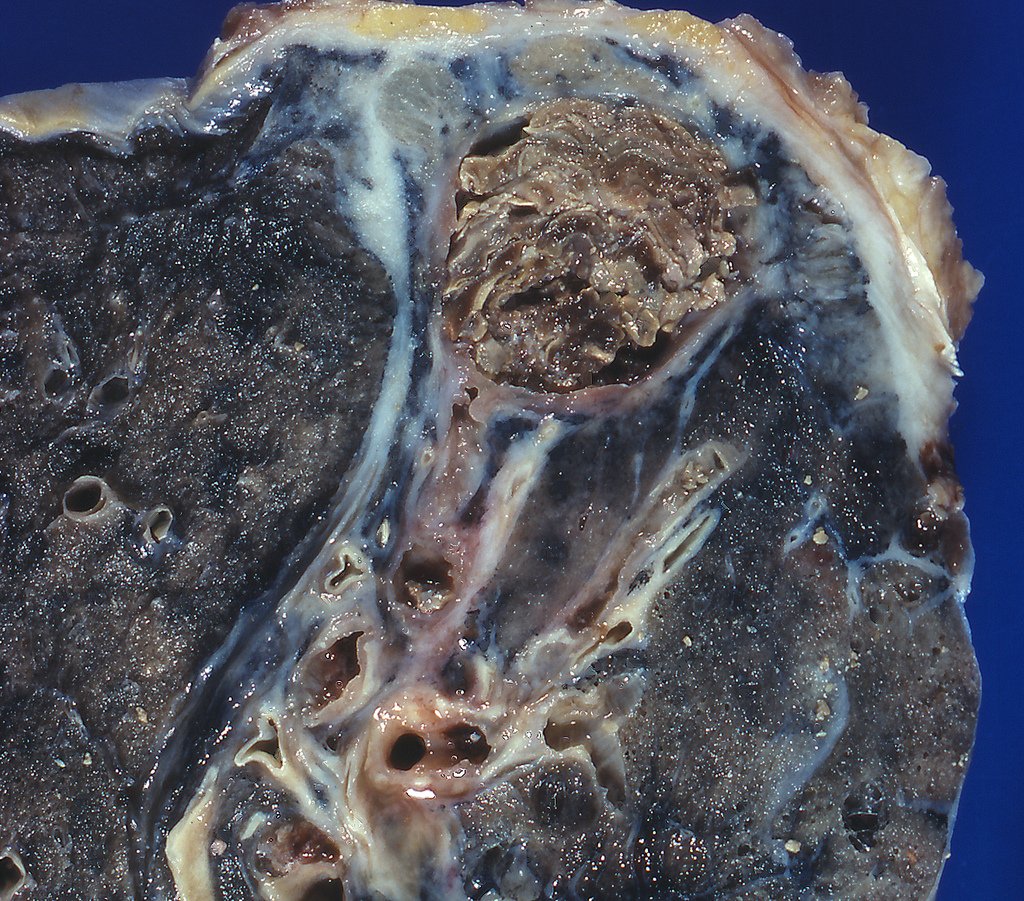
The symptoms of Aspergillus infection can be sneaky and easily mistaken for more common illnesses. Persistent coughing, sometimes producing blood, chest pain, fever, and shortness of breath are common early signs. In severe cases, the infection can destroy lung tissue, leading to cavities or masses known as aspergillomas. These fungal balls can cause significant bleeding and breathing difficulties. Because the symptoms often resemble those of pneumonia or tuberculosis, diagnosis can be delayed, giving the fungus more time to wreak havoc. It’s a chilling reality that what seems like a stubborn cold could be something far more sinister lurking deep within.
The Science Behind the Attack
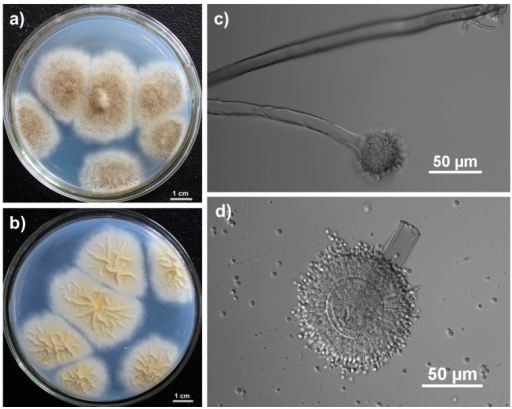
The way Aspergillus attacks is both fascinating and disturbing. Once inside the lungs, the fungus releases enzymes that break down cell walls, allowing it to penetrate and digest living tissue. This process not only provides nutrients for the fungus but also causes inflammation, scarring, and—if unchecked—irreparable damage. The immune response itself can add to the chaos, as the body’s desperate attempt to fight off the invader leads to further swelling and tissue destruction. Scientists are racing to understand exactly how Aspergillus evades the immune system, hoping to develop better treatments and prevention strategies for those most at risk.
Different Faces of Aspergillus Infection

Aspergillus doesn’t cause just one kind of illness. Its impact ranges from mild to life-threatening. Allergic bronchopulmonary aspergillosis (ABPA) triggers severe allergic reactions, often in people with asthma. Aspergilloma, the so-called “fungus ball,” forms when the mold grows in existing lung cavities, leading to coughing and sometimes massive bleeding. The most severe form, invasive aspergillosis, occurs when the fungus spreads rapidly, destroying lung tissue and even moving into the bloodstream. This form is often deadly without aggressive treatment and typically affects the most vulnerable patients. Each type of infection tells its own story, but all share the same sinister protagonist.
Diagnosis: Unmasking the Hidden Invader
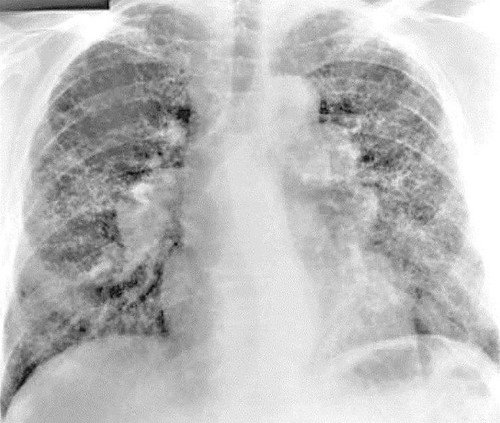
Diagnosing an Aspergillus infection can be like solving a puzzle. Doctors look for clues in a patient’s symptoms, medical history, and risk factors. Imaging tests like chest X-rays and CT scans may reveal suspicious shadows or cavities in the lungs. Laboratory tests are crucial—samples of blood, sputum, or even tissue biopsies are examined for the telltale signs of fungal growth. Sometimes special blood tests can detect antigens or antibodies specific to Aspergillus, helping confirm the diagnosis. The challenge is that these tests are not always definitive, and time is often of the essence. Swift and accurate diagnosis is essential to give patients the best chance at recovery.
Treatment: Fighting Back Against the Fungal Foe
Treating Aspergillus infections is a race against time. Antifungal medications, such as voriconazole or amphotericin B, become the frontline soldiers in this battle. These drugs are powerful but can come with serious side effects, especially when used for long periods. In some cases, surgery may be needed to remove fungal balls or damaged tissue. Treatment is often complicated by the patient’s underlying health problems, making recovery a delicate balance. The real challenge lies in catching the infection early and tailoring therapy to the individual’s needs. It’s a sobering reminder of how a seemingly harmless fungus can turn deadly when given the right opportunity.
Prevention: Protecting Yourself and Your Loved Ones
For most healthy people, avoiding Aspergillus is as simple as breathing. But for those at high risk, prevention becomes a daily concern. Hospitals and care facilities use high-efficiency air filters and strict cleaning protocols to reduce airborne spores. Patients undergoing chemotherapy or transplants may be advised to wear masks, avoid gardening, or steer clear of dusty environments. Education and awareness play key roles—knowing the risks and taking precautions can make all the difference. Simple steps, like keeping indoor spaces clean and well-ventilated, may help lower the risk of exposure in everyday life.
The Role of Climate and Environment
Fungal infections like those caused by Aspergillus are influenced by where we live and how our environment changes. Warm, humid climates support mold growth, making certain regions more prone to outbreaks. Extreme weather events, such as floods or storms, can release massive amounts of spores into the air, increasing risk for vulnerable populations. Urban development and agricultural practices also play a part, disturbing soil and organic material where Aspergillus thrives. As climate change reshapes the world around us, scientists worry that fungal diseases could become more common, affecting new areas and more people than ever before.
Nature’s Double-Edged Sword
While Aspergillus can be deadly under the right conditions, it also plays a crucial role in our ecosystem. It breaks down organic material, recycles nutrients, and even helps produce life-saving medications like antibiotics and immunosuppressants. This dual nature reminds us that what can harm us can also heal us, depending on the context. The challenge lies in harnessing the benefits while minimizing the risks, a delicate balance that scientists and doctors constantly strive to maintain. It’s an awe-inspiring example of how nature operates on a knife’s edge—capable of both creation and destruction.
A Glimpse Into the Future: New Threats and Hope
Researchers are working tirelessly to find better ways to detect and treat Aspergillus infections. Advances in genetic testing and imaging are making earlier, more accurate diagnoses possible. New antifungal drugs are in development, aiming to be more effective with fewer side effects. But the growing problem of drug resistance poses a significant threat, as some strains of Aspergillus become harder to kill. Ongoing research into vaccines and preventive therapies offers hope, especially for those most at risk. The battle is far from over, but every step forward brings us closer to tipping the balance in our favor.
Aspergillus may be an invisible enemy, but its story is a powerful reminder of the hidden dangers that surround us—and the resilience of those who fight back against the odds. How much do we really know about the microscopic world we breathe in every day?