Ever wondered why you get butterflies in your stomach when nervous, or why stress seems to mess with your digestion? These aren’t just old sayings – they reflect a profound scientific reality that researchers are only now beginning to understand. Your gut and brain are engaged in constant conversation, creating what scientists call the gut-brain axis. This connection runs so deep that your digestive system houses more neurons than your spinal cord and produces roughly ninety percent of your body’s serotonin, the so-called happiness hormone. What’s truly fascinating is how this relationship works both ways. Just as your mental state can trigger stomach issues, the trillions of microorganisms living in your gut can influence your mood, anxiety levels, and even your ability to think clearly. Recent breakthroughs in neuroscience and microbiology are revealing that conditions like depression and anxiety might have more to do with what’s happening in your digestive tract than anyone previously imagined. So let’s dive into this remarkable connection that’s revolutionizing how we think about mental wellness.
The Hidden Network Inside Your Digestive System
Deep within the walls of your digestive tract lies what scientists affectionately call your “second brain” – a complex network known as the enteric nervous system. The ENS is two thin layers of approximately 500 million nerve cells lining your gastrointestinal tract from esophagus to rectum. While this gut brain can’t balance your checkbook or write poetry, it orchestrates the intricate dance of digestion with remarkable independence.
This internal command center controls everything from the rhythmic contractions that move food through your system to the precise release of digestive enzymes. Its main role is controlling digestion, from swallowing to the release of enzymes that break down food to the control of blood flow that helps with nutrient absorption to elimination. What makes this system extraordinary is its ability to function autonomously while maintaining constant communication with the brain in your head.
The Two-Way Highway Between Gut and Brain
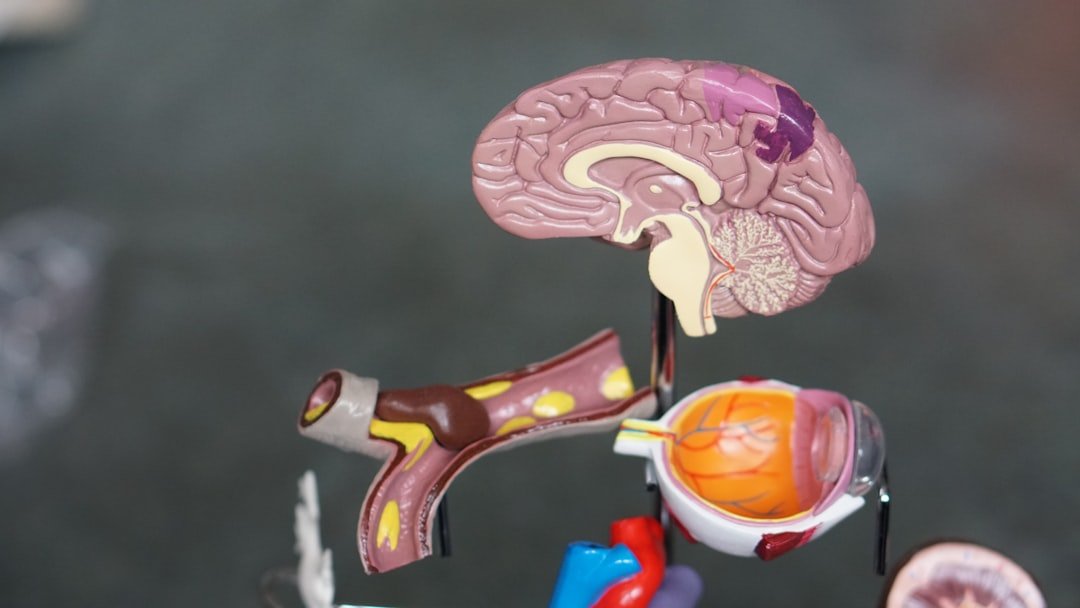
Through direct signals from the vagus nerve, which connects the brain and the gut, as well as through molecules secreted into the bloodstream from our gut microbes and immune cells that traffic from the gut to the rest of the body, our brains and our digestive tracts are in constant communication. This biological superhighway ensures that your mental state can instantly affect your gut, and vice versa.
The communication doesn’t stop at nerve signals. In fact, 90% of serotonin, a mood-boosting hormone, is created in the gut and then travels to the brain. This means your digestive system literally manufactures the chemicals that influence your emotional well-being. When this production goes awry, the effects ripple throughout your entire nervous system, potentially triggering mood disorders and cognitive issues.
The Microbial Universe Influencing Your Mind

Your gut houses roughly one hundred trillion microorganisms – bacteria, viruses, and fungi that collectively weigh about as much as your brain. These tiny residents aren’t passive passengers; they’re active participants in your story. Besides short-chain fatty acids and bile acids, recent studies show that the metabolites produced by the gut microbiota also include some neurotransmitters such as glutamate, GABA, serotonin, and dopamine.
Gut bacteria play an important role in the digestion of food, immune activation, and regulation of entero-endocrine signaling pathways, but also communicate with the central nervous system (CNS) through the production of specific metabolic compounds, e.g., bile acids, short-chain fatty acids (SCFAs), glutamate (Glu), γ-aminobutyric acid (GABA), dopamine (DA), norepinephrine (NE), serotonin (5-HT) and histamine. These bacterial biochemists are essentially running their own neurotransmitter factory right in your digestive tract.
When Stress Wreaks Havoc on Your Gut Ecosystem
The relationship between stress and gut health creates a vicious cycle that can trap people in patterns of poor mental and physical health. Psychological stress has been shown to impact the makeup of the gut microbiome, either indirectly (stressed people may turn to comfort food-heavy diets which in turn change their microbiome makeups) or directly through molecular signals that travel from the brain to the gut and cause certain bacterial species to grow and divide and others to die back.
Stress is often linked to “pro-inflammatory” bacterial species in the gut. This inflammation doesn’t stay confined to your digestive system – it can trigger a cascade of immune responses that affect brain function. The result is often a downward spiral where stress damages your gut microbiome, which in turn produces inflammatory compounds that worsen anxiety and depression, creating even more stress.
The Depression Connection Hidden in Your Digestive Tract

Scientists have discovered that people with depression often show distinct patterns in their gut microbiome composition. GABA is largely produced by Bacteroides in the gut microbiota, and correlation analysis of 16S rRNA sequencing and fMRI data shows that the relative abundance of Bacteroides in the feces of patients with depression is negatively correlated with brain symptoms of depression. When these beneficial bacteria decline, so does the production of calming neurotransmitters.
Recent research highlights the association between gut dysbiosis and psychiatric disorders, including anxiety, depression, and stress-related conditions. Key findings indicate that altered microbial diversity, decreased short-chain fatty acid (SCFA) production, and increased neuroinflammation contribute to disturbances. This discovery has opened entirely new avenues for understanding and treating conditions.
How Anxiety Lives in Your Gut

The connection between gut health and anxiety runs deeper than most people realize. Many GI conditions impact serotonin creation, which explains why 40-90% of people with IBS also have some degree of anxiety or depression. This isn’t coincidental – it reflects the intimate relationship between digestive function and emotional regulation.
There’s a significant overlap among people who have functional gastrointestinal disorders, like IBS (irritable bowel syndrome), and who have disorders, like anxiety. The gut’s inflammatory response to stress can trigger anxiety symptoms, while anxiety can worsen digestive problems, creating a self-perpetuating cycle that’s difficult to break without addressing both components.
Neurodegenerative Diseases and the Gut Connection
Perhaps one of the most surprising discoveries in recent years is how gut health relates to neurodegenerative diseases like Parkinson’s. In Parkinson’s disease, a neurodegenerative condition that affects motor neurons in the brain, gut issues such as constipation and heartburn precede movement symptoms by years or even decades. This suggests that the disease process may actually begin in the digestive system.
And a 2024 study from Harvard researchers found that damage to the upper digestive tract, as with GERD or chronic ulcers, increases the risk of developing Parkinson’s disease years down the road. These findings are revolutionizing how scientists think about the origins of brain diseases, pointing to the gut as a potential early warning system and treatment target.
The Promise of Probiotic Interventions

The emerging science of psychobiotics – live bacteria that provide benefits – offers new hope for treating mood disorders. Probiotics yielded small but significant effects for depression (d = -.24, p < .01) and anxiety (d = -.10, p = .03). Sample type was a moderator for probiotics and depression, with a larger effect observed for clinical/medical samples (d = -.45, p < .001) than community ones.
Notably, in our study probiotic effects were only significant in a subsample with high compliance and accentuated in the follow-up after eight weeks, indicating a remission rate of 55% in the probiotics group compared to a 40% remission rate in the placebo group. These results suggest that carefully targeted probiotic interventions could serve as valuable adjuncts to traditional treatments.
Revolutionary Treatment Approaches on the Horizon

The gut-brain connection is inspiring entirely new therapeutic approaches that target both ends of this biological axis simultaneously. Healthcare providers are beginning to approach these conditions from both sides of the gut-brain axis. You can, too, by taking care of your and gut health. This integrative approach represents a fundamental shift from treating symptoms in isolation to addressing root causes.
Probiotics could provide a non-drug-based approach in the treatment of mood disorders which could help expand the therapeutic options of both psychiatric and non-psychiatric patients, whilst simultaneously being safe and well tolerated. In addition, as they are nutritional supplements, probiotics could help alleviate the social stigma faced by people taking psychotropic medication. This could democratize treatment and make interventions more accessible to people who might otherwise avoid seeking help.
Conclusion
The gut-brain connection represents one of the most exciting frontiers in research, fundamentally changing how we understand conditions like depression and anxiety. Rather than viewing these disorders as purely brain-based problems, we now recognize that mental wellness depends on the delicate balance of trillions of microorganisms living in our digestive system. This discovery offers genuine hope for millions of people struggling with issues. By nurturing our gut microbiome through targeted interventions – whether through specific probiotics, dietary changes, or stress management techniques – we may be able to influence our mental state in ways that were previously unimaginable. The future of treatment likely lies not just in addressing the brain, but in healing the entire gut-brain axis. What fascinates you more – the idea that your gut bacteria are producing mood-regulating chemicals, or that digestive problems might predict brain diseases decades before symptoms appear? Share your thoughts in the comments below.




