It sounds like folklore: a twist in the genetic code that lets a few people shrug off heat that would buckle the rest of us. In labs and burn units, though, a quieter story is unfolding, one that swaps myths for molecules and replaces invincibility with nuance. There is no single switch that makes a person truly impervious to flames, yet certain gene variants do appear to raise thresholds for heat pain, curb runaway inflammation, or speed the repair of damaged skin. That trio – sensing, damage, recovery – can look a lot like resilience, especially in extreme environments. Think of it as a mosaic of advantages rather than a magic shield, and suddenly the science stops sounding supernatural and starts sounding urgent.
The Hidden Clues

The Hidden Clues (image credits: wikimedia)
I remember edging too close to a campfire as a kid, the heat pulsing like a living thing against my shins, and wondering how anyone could ever walk across coals. Years later, the lab answer is less theatrical and more interesting: people vary, deeply, in how their nerves sense heat, how their skin holds the line, and how their immune system cleans up the mess.
Clinicians see the clues in rare patients who barely register heat pain yet still suffer burns – and heal in distinctive ways. Researchers see them in volunteers whose heat-pain thresholds sit a notch higher than average, or whose blisters resolve faster after the same insult. To call such people fireproof is a stretch, but measurable edges exist, tucked in the wiring of pain sensors, the scaffolding of the skin barrier, and the body’s damage-control chemistry. Follow those edges and you find candidate genes hiding in plain sight.
From Ancient Tools to Modern Science

Firewalking and ember rituals once looked like proof of human heat immunity, but physics and practice explain most of the spectacle: low thermal conductivity of coals, swift steps, and dry skin buy seconds of safety. Modern science asks a different question – why do some people still tolerate more heat, or recover faster, even when the physics is the same?
Enter genome-wide scans, exome sequencing, and careful pain-threshold testing with heated probes. These tools trace differences to ion channels, barrier proteins, and stress-response switches. Put simply, engineers would call it a systems problem: sensors, structure, and emergency protocols. The story is less about walking on fire and more about how bodies walk away from it.
The Biology of Heat and Pain

Heat pain starts at the skin’s front line, where ion channels such as TRPV1 and its cousins sit like microscopic thermometers on nerve endings. When temperatures climb into the uncomfortable range, those channels open, sending electrical alarms that feel like searing pain and trigger protective reflexes.
Beyond nerves, keratinocytes – the main skin cells – don’t just stand there; they signal, recruit immune cells, and help rebuild the barrier. Blood vessels widen to carry heat away and ferry in repair crews, while sweat glands join the cooling effort. If this choreography is a beat faster or a shade calmer because of genetics, burns can be less deep and healing more complete. A person isn’t immune to fire; they’re better at not letting heat run the table.
- Heat sensing depends on ion channels that set individual pain thresholds.
- Skin-barrier proteins and lipids influence how fast heat penetrates tissue.
- Inflammation and antioxidant responses shape damage and recovery over hours and days.
The Mutation Candidates

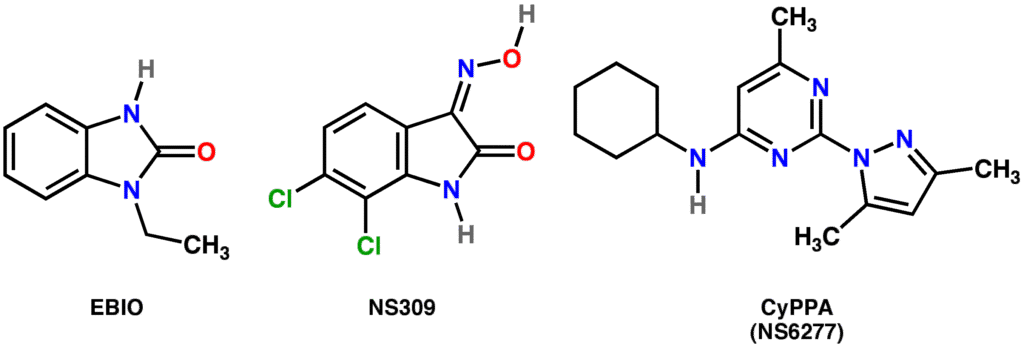
Start with the sensors: variants in SCN9A and PRDM12 are known to blunt pain broadly in rare conditions, which can tragically invite unnoticed injuries. More subtle differences in TRPV1 and related channels can nudge heat-pain thresholds without erasing them, offering a modest cushion rather than a superpower.
Shift to the barrier: genes like FLG, which encodes filaggrin, influence how tightly the outer skin layers lock together and retain moisture, factors that affect heat transfer and blistering. And in the cleanup crew, regulators such as NFE2L2 (also called NRF2) help marshal antioxidant defenses; certain variants appear to tune how vigorously cells respond to oxidative stress after a burn. Layer in heat-shock proteins – molecular chaperones that refold stressed proteins – and you get a plausible recipe for resilience: sense a bit less, leak a bit less, recover a bit faster. None of this equals immunity, but in risk terms, small genetic shoves matter.
Why It Matters

Burn care has long focused on prevention, rapid cooling, and skilled wound management – and rightly so. Genetic insight doesn’t replace those pillars; it strengthens them by explaining why two people with similar injuries can diverge in pain, scarring, or infection risk.
Clinically, understanding the pathways behind heat pain and repair could steer smarter analgesics and targeted anti-inflammatory care. Public health-wise, it could flag workers who need extra protection in high-heat jobs, or identify those who might safely tolerate certain tasks with standard gear. The broader scientific payoff is clarity: when a myth like fireproof humans dissolves, it reveals testable biology we can actually use. In that sense, the hype has been hiding a more valuable truth.
- Traditional methods: one-size-fits-all equipment and protocols.
- Genetics-informed methods: personalized risk profiles and tailored recovery plans.
- Outcome goal: fewer severe burns, faster healing, and better long-term function.
Global Perspectives
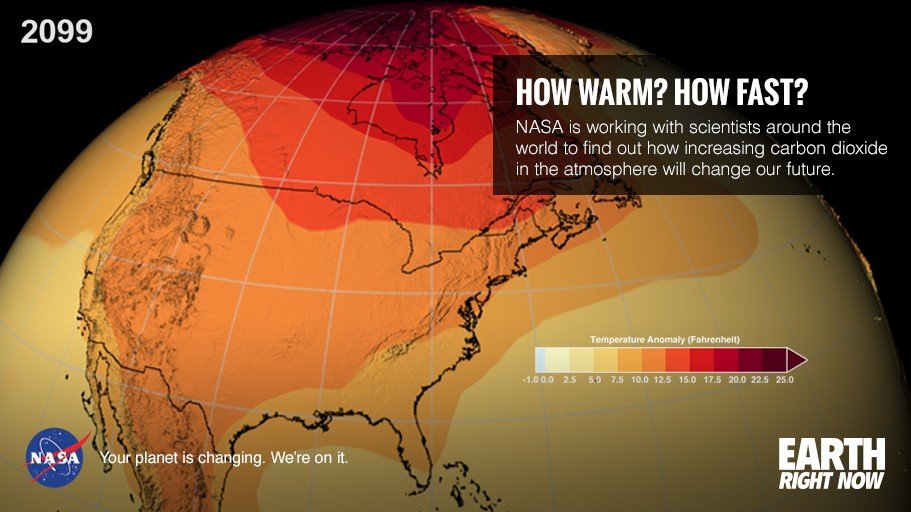
Around the world, communities face different heat hazards – wildfires in the American West, industrial heat in South Asia, and urban heat waves almost everywhere. Population genetics also varies, shaping skin physiology, sweating patterns, and inflammatory tendencies that interact with climate and work.
Skin pigmentation, for example, profoundly alters ultraviolet risk but does less for direct thermal burns, so behavioral and environmental factors still dominate. Occupational culture matters too: training, hydration habits, and protective gear can easily outweigh any genetic nudge. The takeaway is pragmatic and a bit humbling – biology offers small levers, but context pulls the biggest ones. Even so, mapping those levers could make global burn prevention more precise.
The Future Landscape
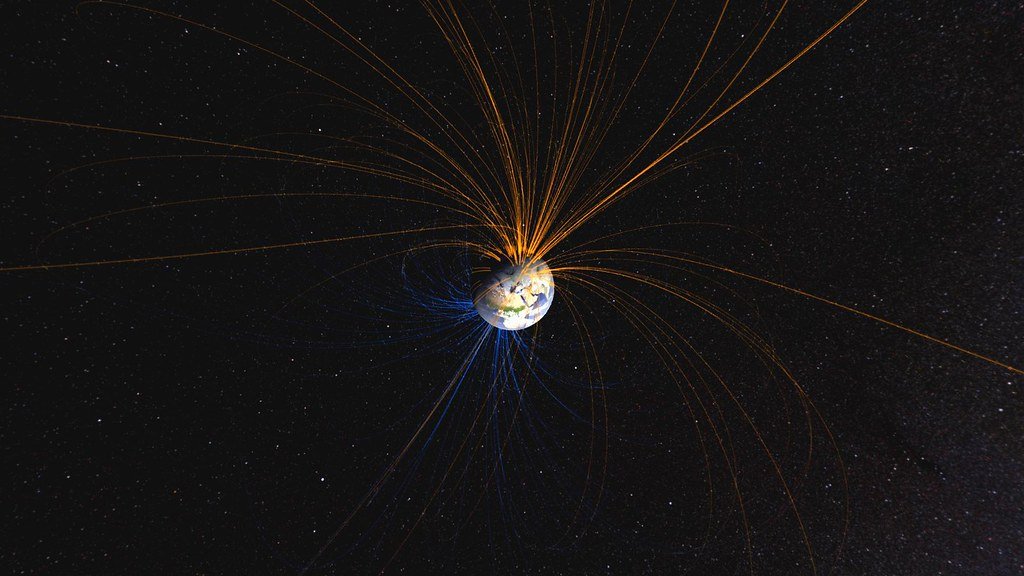
The Future Landscape (image credits: wikimedia)
On the horizon, researchers are testing topical TRPV1 modulators that dull heat pain without numbing touch, and biomaterials that mimic heat-shock responses to protect cells during the first critical hours after injury. Noninvasive sensors that track skin temperature, perfusion, and inflammatory markers could guide field decisions in real time.
Farther out, precision medicine may combine genotyping with occupational screening to put the right gear on the right person at the right moment. Gene editing to harden humans against heat is neither realistic nor ethical as a population strategy, but boosting endogenous stress responses – temporarily and locally – looks plausible. Expect setbacks, because biology is messy and trade-offs are real: dampen inflammation too much and you invite infection; blunt pain too far and you invite harm. The winning solutions will be tuned, temporary, and targeted.
The Hidden Costs of Being “Resistant”

There’s a paradox here that’s easy to miss: people who feel less heat pain may take bigger risks, and that can end badly. Pain, annoying as it is, protects; edit it too much and the guardrail disappears.
Likewise, a robust inflammatory response causes swelling and redness that look alarming, but it also clears debris and pathogens. Skew the system toward calm, and healing can stall. This is where genetics helps us hold two ideas at once – some pathways are good to dampen for a few hours, others need to roar briefly and then quiet. The art is knowing which is which, and when.
Conclusion

If this research sparks your curiosity, start close to home: audit your space for burn risks, swap out frayed cords, and keep a timer near the stove. In wildfire regions, make defensible space around homes, pack go-bags, and learn local evacuation routes before smoke appears on the horizon.
Support the people at the sharp end of heat – firefighters, field researchers, and clinicians – by backing community funds and burn centers that advance both care and science. If a clinical trial for new burn treatments is recruiting in your area and you’re eligible, consider volunteering; small studies become big advances when ordinary people say yes. Most of all, keep a steady skepticism toward magical claims and a steady faith in careful biology – because progress here won’t look like invincibility, it will look like fewer tragedies and faster recoveries. Would you have guessed that the most powerful kind of fireproofing starts with understanding pain, not denying it?

Suhail Ahmed is a passionate digital professional and nature enthusiast with over 8 years of experience in content strategy, SEO, web development, and digital operations. Alongside his freelance journey, Suhail actively contributes to nature and wildlife platforms like Discover Wildlife, where he channels his curiosity for the planet into engaging, educational storytelling.
With a strong background in managing digital ecosystems — from ecommerce stores and WordPress websites to social media and automation — Suhail merges technical precision with creative insight. His content reflects a rare balance: SEO-friendly yet deeply human, data-informed yet emotionally resonant.
Driven by a love for discovery and storytelling, Suhail believes in using digital platforms to amplify causes that matter — especially those protecting Earth’s biodiversity and inspiring sustainable living. Whether he’s managing online projects or crafting wildlife content, his goal remains the same: to inform, inspire, and leave a positive digital footprint.