Rogue Defenders Accelerate ALS Destruction (Image Credits: Images.newscientist.com)
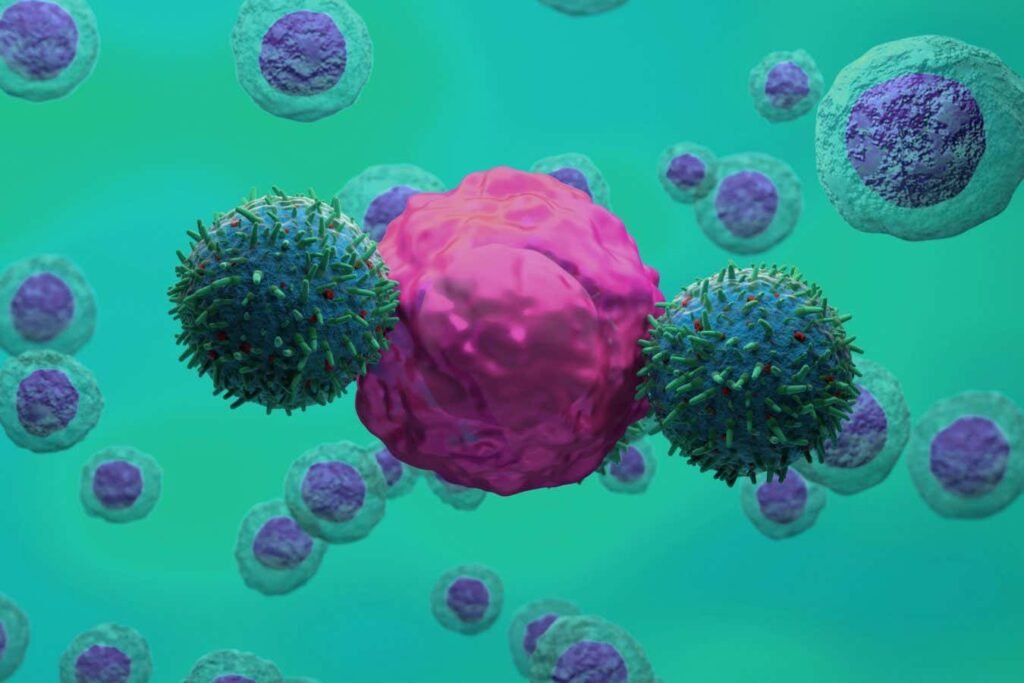
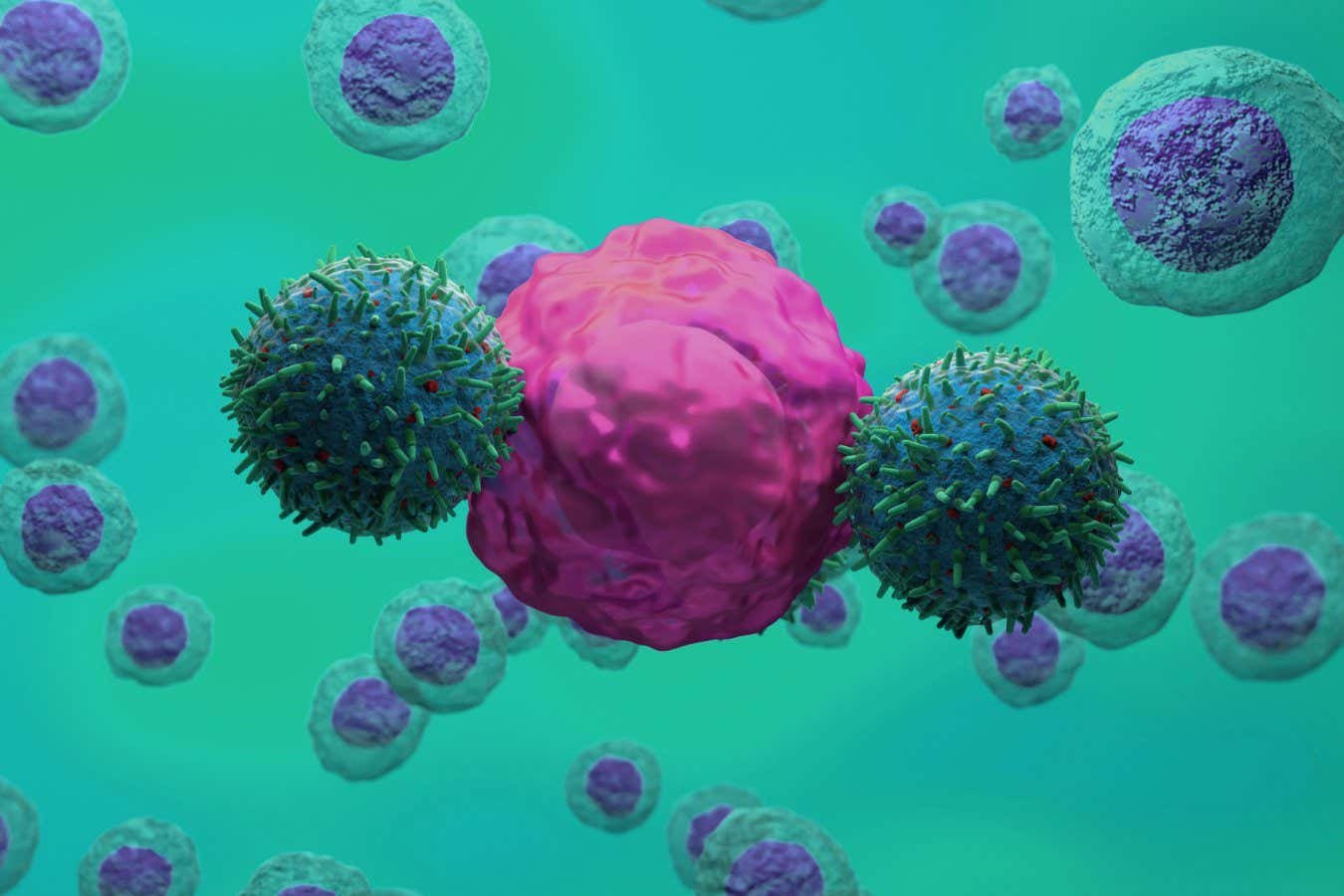
Researchers unveiled a novel CAR-T cell therapy designed to neutralize overzealous immune cells fueling the destruction of motor neurons in amyotrophic lateral sclerosis (ALS).[1]
Rogue Defenders Accelerate ALS Destruction
Microglia, the brain’s resident immune cells, play a critical role in defending against threats and clearing debris. In ALS patients, however, these cells shift into a hyperactive state, stripping away excessive synapses and hastening neuron death. Davide Trotti at the Jefferson Weinberg ALS Center in Pennsylvania described them as becoming “out of control.”[1]
This inflammation contributes significantly to the disease’s progression, where motor neurons controlling voluntary muscles degenerate relentlessly. Patients typically face a life expectancy of two to five years post-diagnosis, with few effective treatments available for the most common sporadic forms. Trotti’s team sought to intervene by identifying a specific marker on these damage-amplifying microglia.
Zeroing In on the uPAR Marker
Analysis of brain and spinal cord tissue from ALS patients revealed elevated levels of urokinase-type plasminogen activator receptor (uPAR) protein on the surface of harmful microglia. This protein effectively “tagged” the rogue cells, distinguishing them from healthy ones. “So they are tagged, and knowing the tag, we can go after them and remove them from the central nervous system,” Trotti explained.[1]
The discovery stemmed from multiplexed immunofluorescence studies and datasets confirming uPAR’s presence in both sporadic and familial ALS cases, particularly in affected regions.[2] These uPAR-high microglia even induced neurite retraction in lab-grown neurons, underscoring their destructive potential.
Engineering Precision Immune Assassins
Leveraging technology proven in cancer treatments, scientists genetically modified T cells into CAR-T cells equipped to recognize and destroy uPAR-expressing microglia. In cell culture experiments, these engineered cells eliminated the overactive microglia with over 80% efficiency while sparing neurons and resting microglia.[2]
The third-generation CAR-T design incorporated an anti-uPAR single-chain variable fragment for targeted cytolysis. This specificity addressed a key challenge in neurodegeneration: avoiding broad immune suppression that could worsen outcomes.
- Targets only uPAR-positive pathogenic microglia.
- Demonstrated antigen-dependent killing in stimulated human microglia models.
- Preserved healthy brain cells in mixed cultures.
- Built on CAR-T success against blood cancers and autoimmune diseases.
Toward Human Trials and Wider Impact
Mouse models carrying ALS-causing mutations now undergo testing with the uPAR CAR-T cells, with preliminary results expected within a year. Regulators could fast-track human trials if data proves compelling. Ammar Al-Chalabi at King’s College London called the evidence for immune dysfunction in ALS “mounting” and deemed the approach “very promising and interesting.”[1]
Beyond ALS, the strategy holds potential for other conditions like Alzheimer’s, where similar microglial overactivation occurs. Parallel research at Washington University targeted amyloid plaques in Alzheimer’s mouse models, reducing plaques and inflammation.[3] Challenges remain, including CAR-T side effects and high costs, but efforts aim to streamline production.
Key Takeaways:
- CAR-T cells selectively eliminate disease-amplifying microglia via uPAR targeting.
- Cell studies confirm neuron safety and high efficacy.
- Ongoing mouse trials could pave way for ALS human studies soon.
This innovation reframes ALS not just as inevitable neuron loss, but as a battle against misguided immunity – one where precision tools like CAR-T cells might buy precious time. Trotti emphasized that the goal remains slowing progression, not curing it.[1] What are your thoughts on repurposing cancer therapies for brain diseases? Share in the comments.