Imagine a world where a simple break in temperature can decide whether a life-saving vaccine works or not. Picture health workers trekking across scorching deserts, icy mountains, or bustling cities, all the while clutching a small box filled with vials that must stay cold—even when the world outside is anything but. This isn’t science fiction. It’s the everyday reality of moving vaccines from factories to the arms of people all over the globe. The cold chain is the invisible lifeline that keeps vaccines potent, safe, and ready to save lives. But what does it really take to keep this chain unbroken? And why does it matter so much for global health? Let’s peel back the layers on one of the unsung heroes of modern medicine.
The Basics: What Is a Vaccine Cold Chain?
At its core, the vaccine cold chain is a temperature-controlled supply line that moves vaccines from where they’re made to where they’re needed. But it’s not just a simple fridge-to-fridge journey. It’s a carefully managed relay race, where every link—from giant warehouses to remote clinics—must keep vaccines at the right temperature, usually between 2°C and 8°C. If the chain breaks, vaccines can spoil, just like milk left out in the sun. This isn’t just about convenience; it’s about saving lives, because a compromised vaccine might not work, or worse, could be dangerous.
Why Temperature Control Matters So Much

Vaccines are delicate. Many are made with weakened viruses or proteins that can fall apart if they get too hot or cold. Think of them like ice cream on a hot day: once they melt, you can’t refreeze them and expect the same taste—or in this case, the same protection. Even a few hours outside the safe temperature can make a vaccine useless. This is why temperature monitoring is taken so seriously, with alarms, sensors, and logbooks tracking every degree along the way.
The Journey: From Factory to Field

The path a vaccine travels is long and often winding. It begins in ultra-clean factories, where batches are carefully tested and packed. From there, vaccines move to central storage facilities—think massive, cold warehouses humming with generators. They’re loaded onto refrigerated trucks or planes, sometimes crossing continents. At every stop, workers check temperatures and log their readings. The final leg might be on the back of a motorcycle, a donkey, or even a health worker’s backpack. Each stage is a test of both technology and human determination.
Vaccine Types and Their Temperature Needs
Not all vaccines are created equal when it comes to cold. Some, like the oral polio vaccine, are extra sensitive and need near-freezing conditions. Others, such as the newer mRNA COVID-19 vaccines, have famously strict requirements—some needing storage at -70°C, colder than winter in Antarctica. The variety in temperature needs means cold chains must be flexible and incredibly reliable. It’s like juggling eggs, ice cubes, and chocolate bars all at once, each needing their own special handling.
The Science Behind Vaccine Stability

What makes vaccines so fragile? It’s all about their ingredients. Proteins and live viruses can change shape or die when exposed to the wrong temperature. Scientists work hard to make vaccines more stable, sometimes adding special ingredients called stabilizers. But even then, most vaccines still need that careful cold embrace. Without it, their science loses its magic, and the immune system won’t get the training it needs.
High-Tech Tools: Monitoring and Alarms

Modern cold chains use a toolkit that would make any gadget lover jealous. Tiny data loggers ride with vaccine shipments, recording temperatures every minute. If the temperature slips, alarms sound instantly, alerting workers to take action. Some systems use GPS and wireless technology so that supervisors far away can see the health of every box in real-time. These innovations turn the cold chain into a high-tech watchdog, guarding against disaster.
Challenges in Remote and Resource-Poor Settings

In cities, keeping things cold is tough but doable. But in remote villages or conflict zones, it’s a whole different story. Power outages, rough roads, and extreme weather can all threaten the chain. Sometimes, health workers must carry vaccines for hours on foot, using simple insulated bags. In places without reliable electricity, solar-powered fridges or special ice packs become game changers. The people who keep these cold chains running are often unsung heroes, working quietly behind the scenes.
Solar-Powered Fridges and Other Innovations

Necessity breeds invention, and the vaccine cold chain is proof of that. Solar-powered refrigerators have revolutionized vaccine storage in sunny but electricity-poor regions. These fridges use sunlight to keep vaccines safe, even during blackouts. Other innovations include freeze-proof carriers, special cooling gels, and even “smart” vials that change color if they get too warm. Each new tool is a step closer to ensuring every child, no matter where they live, gets a working vaccine.
The Human Element: Training and Dedication

All the tech in the world can’t replace the human touch. Cold chain success depends heavily on the dedication and training of health workers. They need to know exactly how to pack, transport, and store vaccines, often under stressful conditions. Mistakes can be costly, so regular trainings, checklists, and support networks are essential. It’s a job that demands both precision and passion—a rare combination that keeps the chain unbroken.
Global Logistics: Coordinating Across Borders
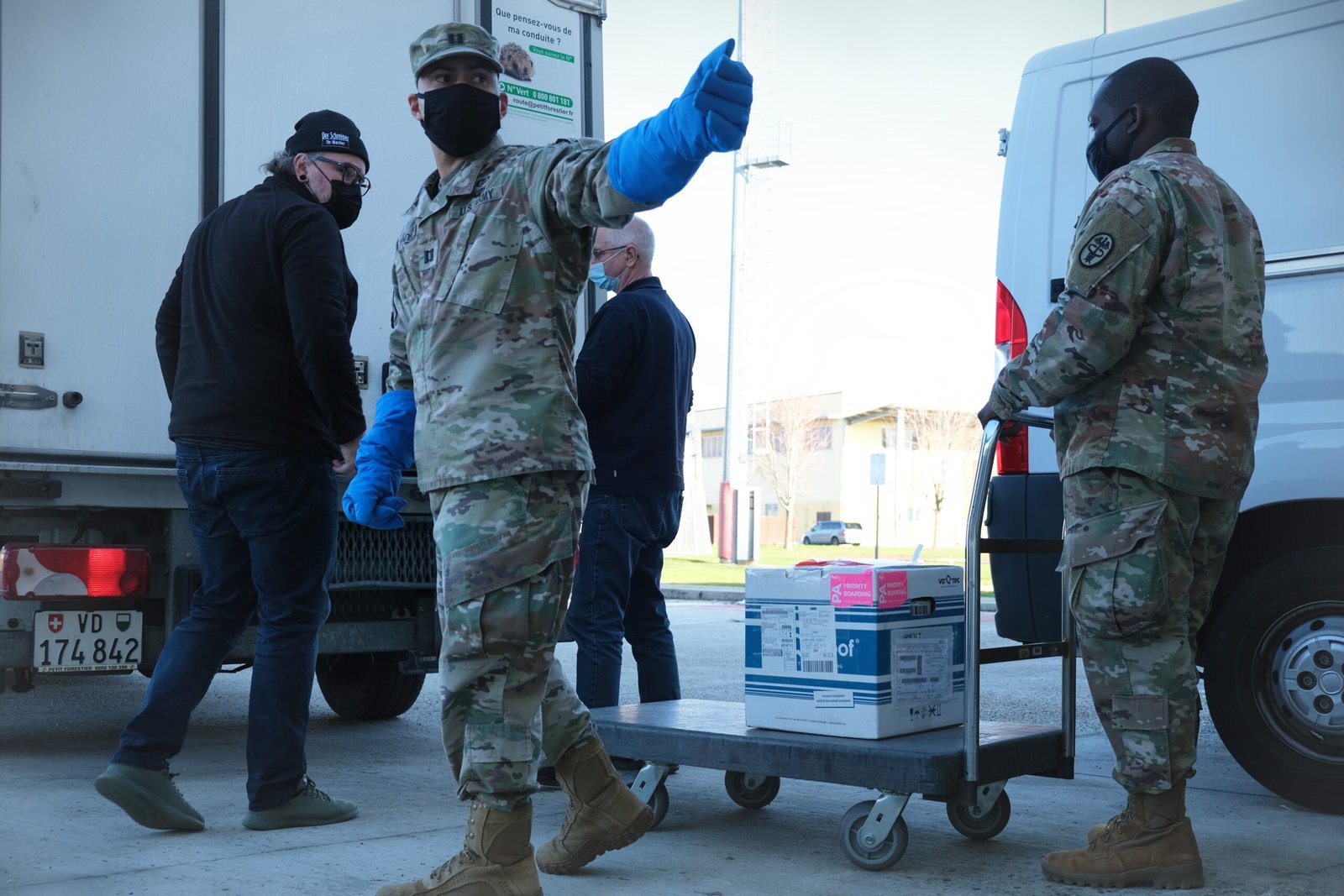
Vaccine cold chains are not just local—they’re global. International agencies, governments, and non-profits must all coordinate to move vaccines smoothly across borders. Customs delays, paperwork, and regulations can cause headaches. It’s a bit like a relay race where each runner speaks a different language. Success depends on trust, clear communication, and a shared mission: getting potent vaccines to people who need them, no matter where they are.
Cold Chain Failures: When Things Go Wrong
Sometimes, despite best efforts, the chain breaks. Maybe a fridge fails overnight, or a shipment is delayed at the airport. When this happens, vaccines may have to be thrown away, wasting precious resources. In the worst cases, people may get shots that don’t work, leaving communities vulnerable. These failures are heartbreaking, but they also drive innovation and improvements—each mistake is a lesson for the future.
The Impact on Immunization Campaigns

Mass vaccination drives, like those against polio or measles, rely on the cold chain running perfectly. If vaccines arrive spoiled, entire campaigns can grind to a halt. This delays protection for millions of people, sometimes sparking new outbreaks. The cold chain isn’t just a technical requirement; it’s a linchpin that holds together the promise of immunization. When it works, it’s practically invisible; when it fails, the consequences are impossible to ignore.
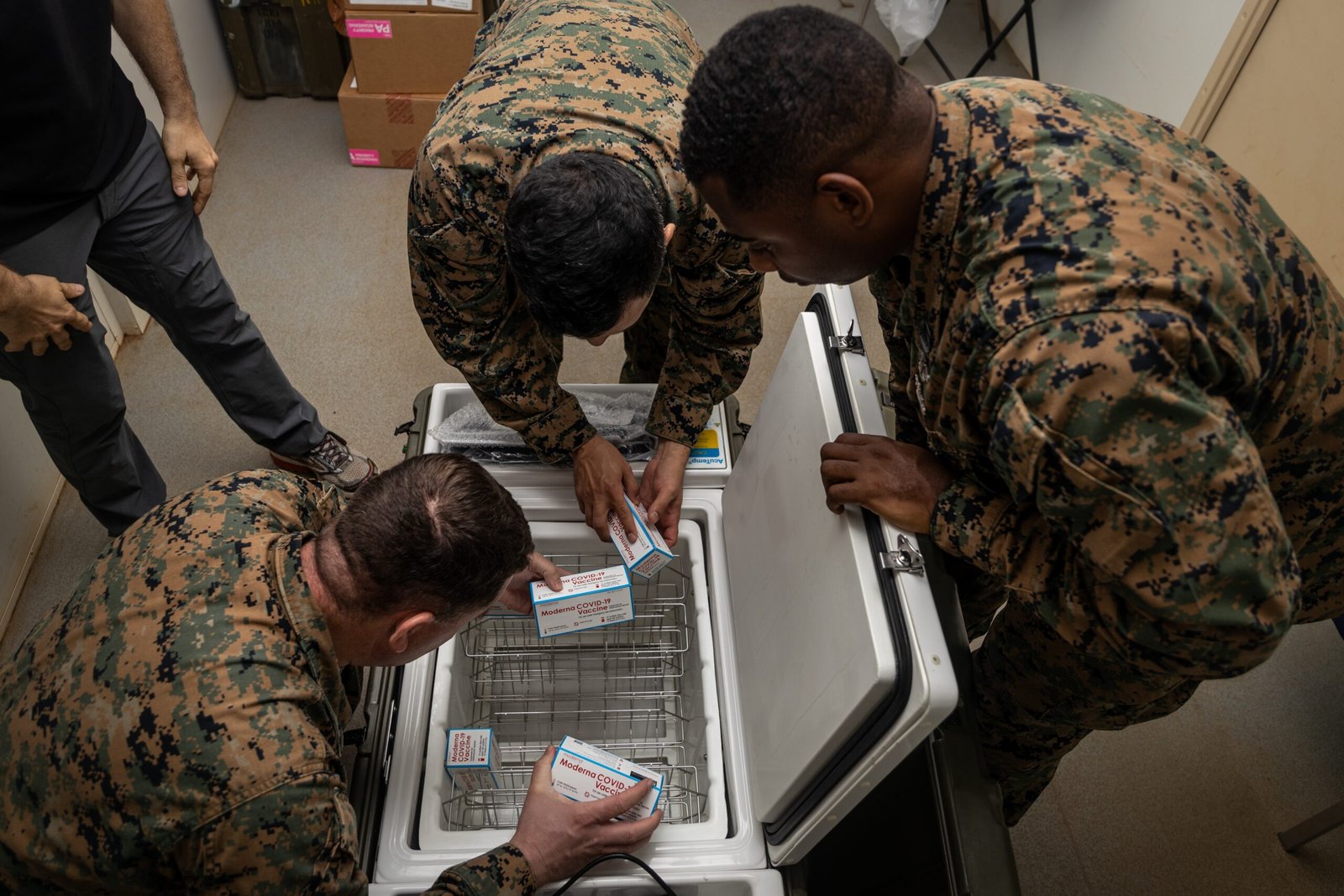
Emergency Response: Cold Chains in Crisis Situations
Natural disasters, wars, and pandemics put extra pressure on cold chains. In emergencies, the need for vaccines skyrockets, but the infrastructure may be damaged or overwhelmed. Rapid-response teams use portable coolers, mobile fridges, and even drones to deliver vaccines to disaster zones. These heroic efforts show just how adaptable and resilient the cold chain can be under pressure, delivering hope when it’s needed most.
Environmental Concerns: Balancing Safety and Sustainability
Running fridges and trucks around the clock takes energy, often from fossil fuels. This creates a dilemma: how to keep vaccines safe without harming the planet. The push for solar-powered fridges, eco-friendly packaging, and efficient logistics is growing. Balancing safety with sustainability is a new frontier for cold chain managers, challenging them to think green while saving lives.
The COVID-19 Pandemic: A Turning Point for Cold Chains

The COVID-19 pandemic threw the cold chain into the global spotlight. The need to deliver billions of vaccine doses—some requiring ultra-cold storage—forced rapid upgrades in infrastructure and technology. The world watched as dry ice, thermal shippers, and global tracking systems became everyday news. Lessons from this crisis are now shaping the future of vaccine delivery, making cold chains smarter, faster, and more resilient than ever.
The Future: Next-Gen Vaccines and Smart Cold Chains

Exciting research is underway to create vaccines that don’t need refrigeration, using freeze-drying or new formulations. Meanwhile, “smart” cold chains with artificial intelligence and automated alerts are on the horizon. The dream? A world where no child misses a vaccine because of a broken fridge. Until then, the cold chain remains a marvel of human ingenuity and a silent guardian of global health.
Why Everyone Should Care About Cold Chains
It’s easy to overlook the cold chain when we roll up our sleeves for a shot. But behind every vaccine is a vast, invisible effort that connects scientists, engineers, health workers, and communities. The cold chain is a testament to what humanity can achieve when we work together for a common good. Next time you get a vaccine, remember the journey it took—and the countless hands that kept it safe, cold, and powerful.



