The story of stress is no longer just about tight shoulders and racing thoughts; it’s a molecular drama that unfolds inside our cells. Scientists are now tracing the fingerprints of stress across DNA switches, power-hungry mitochondria, and vigilant immune sentries, and the plot twists are sobering. What looked like fleeting anxiety can etch lasting marks – tiny edits that tilt biology toward resilience or disease. Yet inside this threat sits opportunity: if we can map the cellular choreography, we can learn to nudge it back into balance. The question is no longer whether stress changes the body, but how far those changes go and how we can steer them.
The Hidden Clues
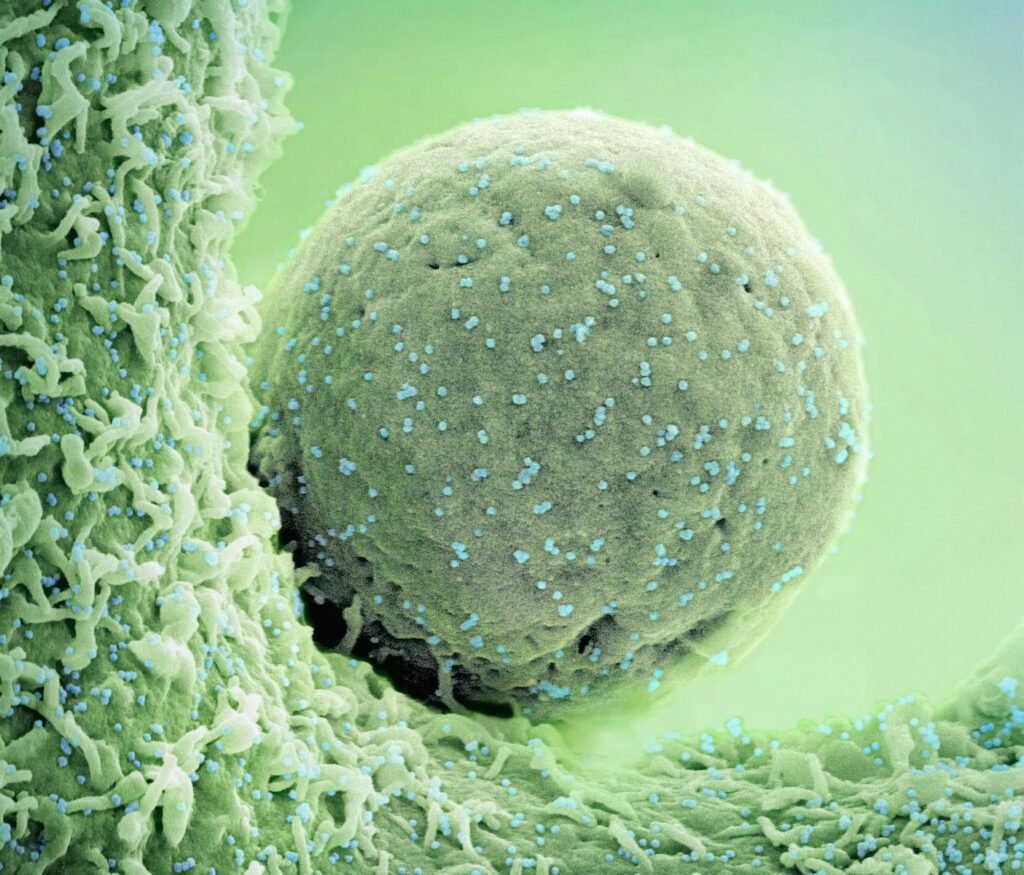
Under a microscope, stress isn’t a vibe; it’s a pattern – proteins folding differently, genes flickering on and off, membranes hardening like winter soil. Cells under pressure release distress signals that ripple through tissues, prompting neighbors to rewire their own behavior. I’ve seen researchers stare at heat maps of gene activity as if reading weather radar before a storm, watching islands of inflammation bloom. Hidden in those color grids are clues to fatigue, pain, and brain fog that people carry for months. It feels strangely intimate, like seeing the body’s private diary.
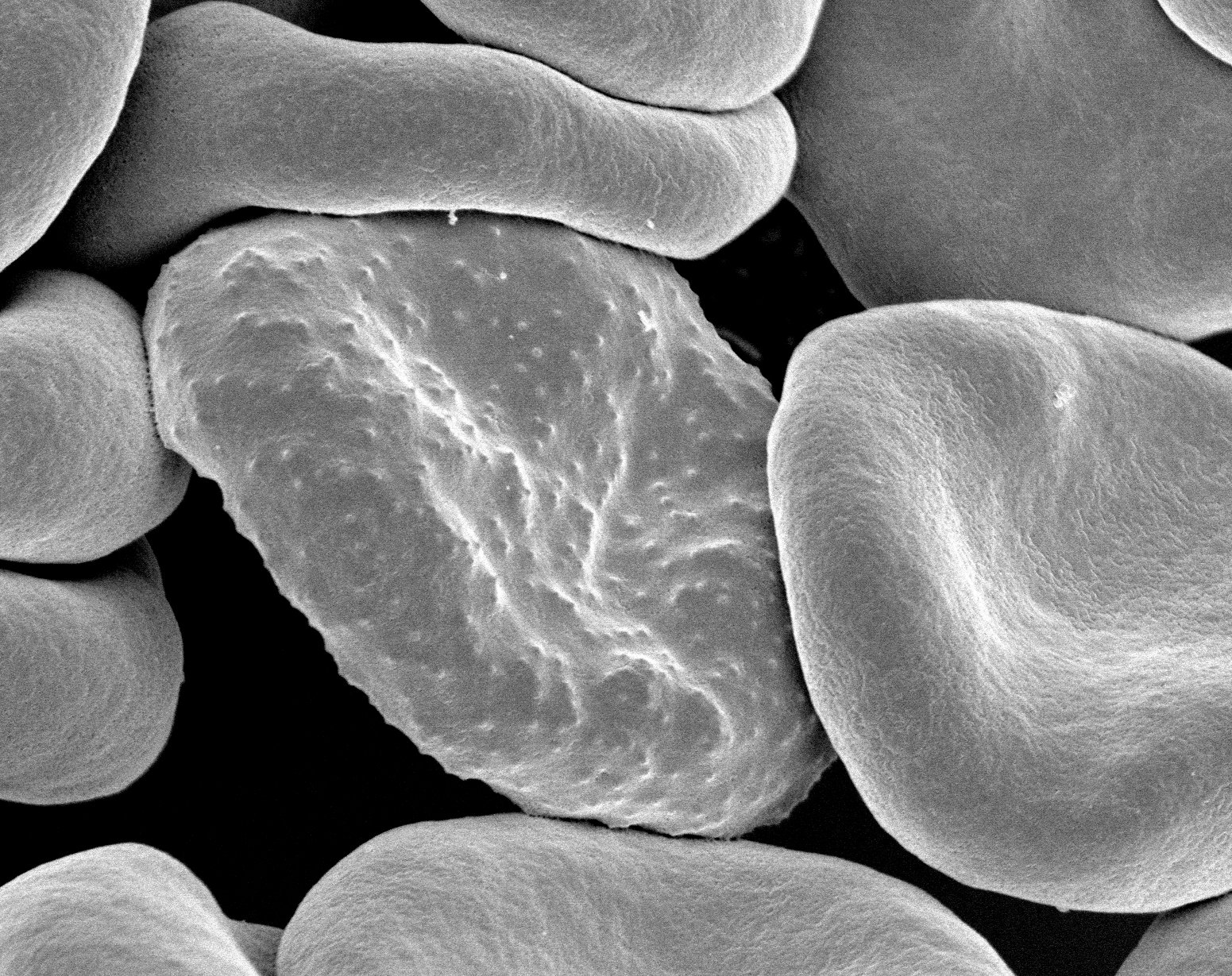
These clues add up across systems. Nerve cells shorten their branches, heart cells change their calcium rhythms, and liver cells switch energy tactics to survive lean times. Even the gut’s microbial tenants shuffle, trading diversity for a siege-ready lineup. When scientists zoom out, the pattern looks like a city shifting to emergency mode – lights on, streets cleared, long-term projects paused. That pause is protective in the short term, but costly when it never ends.
From Ancient Tools to Modern Science

Stress research began with blunt instruments: measure a hormone, watch a rat, draw broad conclusions. Today, scientists wield single-cell sequencing, spatial maps of tissues, and live-cell sensors that track molecular jolts in real time. Instead of averaging signals across millions of cells, they listen to single voices in a crowded room. This evolution is like upgrading from a stethoscope to a satellite array. You hear not just the heartbeat but the choir, the solos, and the off-key notes that predict trouble.
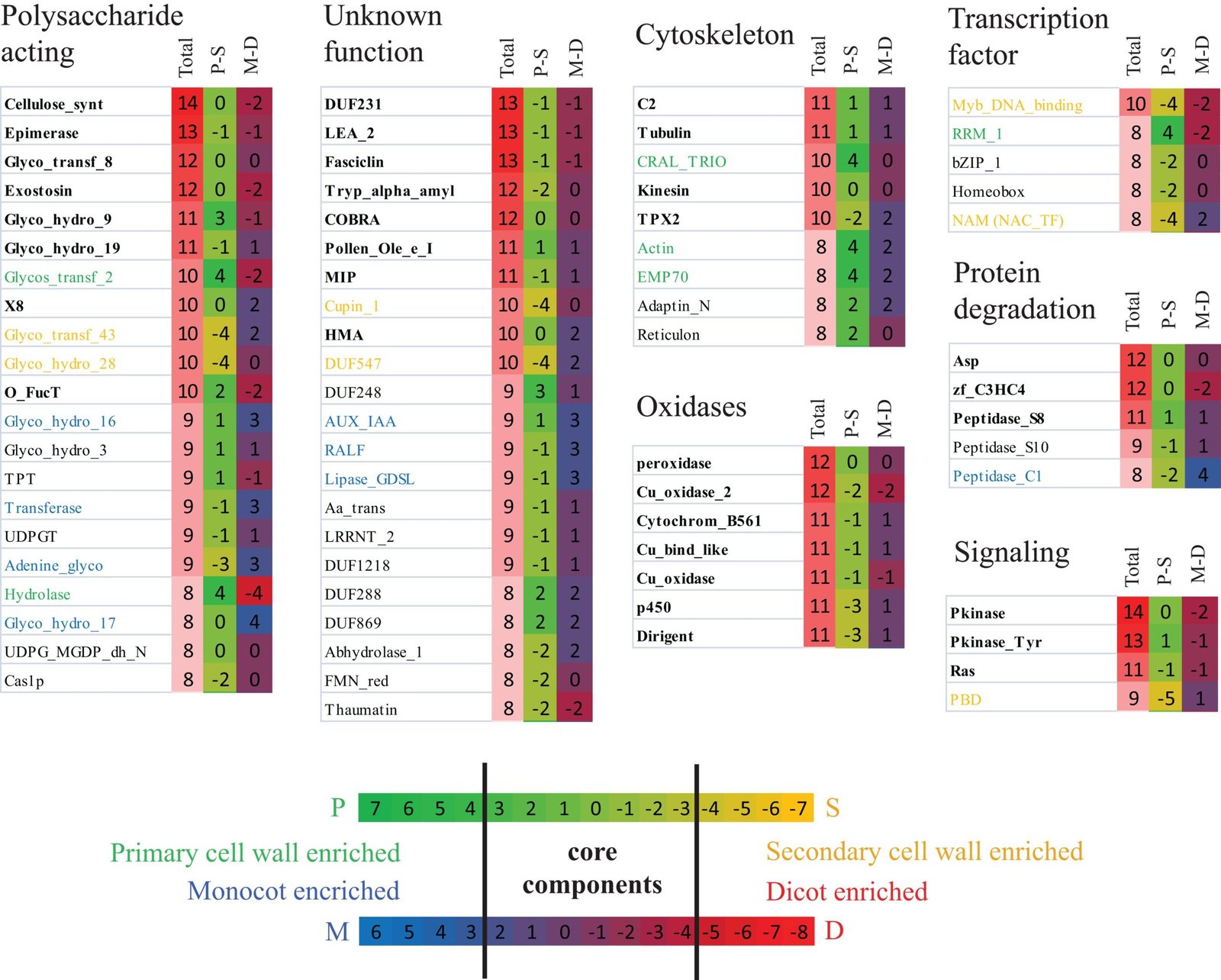
Spatial transcriptomics now pinpoints exactly where stressed cells cluster in organs, revealing hotspots around blood vessels, nerves, and immune hubs. ATAC-seq shows how chromatin opens like a book to be read – or slams shut to stay silent – when threats loom. Proteomics follows the heavy lifters, tracking the wear and tear on molecular machines over weeks, not minutes. Layered together, these tools build a moving portrait that makes stress visible, mappable, and, crucially, testable.
Inside the Stress Response: Hormones, Nerves, and Timers

The body’s alarm starts with signals from the brain’s command center, sending a fast jolt through the sympathetic nerves and a slower wave via stress hormones. Adrenaline primes muscles and heartbeat in seconds, while cortisol reshapes metabolism and immunity over hours. This duet keeps us alive during real danger, but when daily life mimics sirens, the system never fully resets. The circadian clock, meant to keep biology in time with sunrise, drifts out of rhythm. Cells then read mixed instructions: repair now, but also stay on guard.
Those mixed signals seep into cell cycles and protein synthesis, tugging at every process that depends on timing. Some cells become hypersensitive, others numb to the same cues, fracturing coordination across tissues. That fragmentation fuels the feeling of being wired and tired at once – like pressing the gas and brake together. Over time, it’s the mismatch, not just the intensity, that wears the machine down. The body wasn’t built for a fire drill every hour.
Epigenetic Scars and Cellular Memory
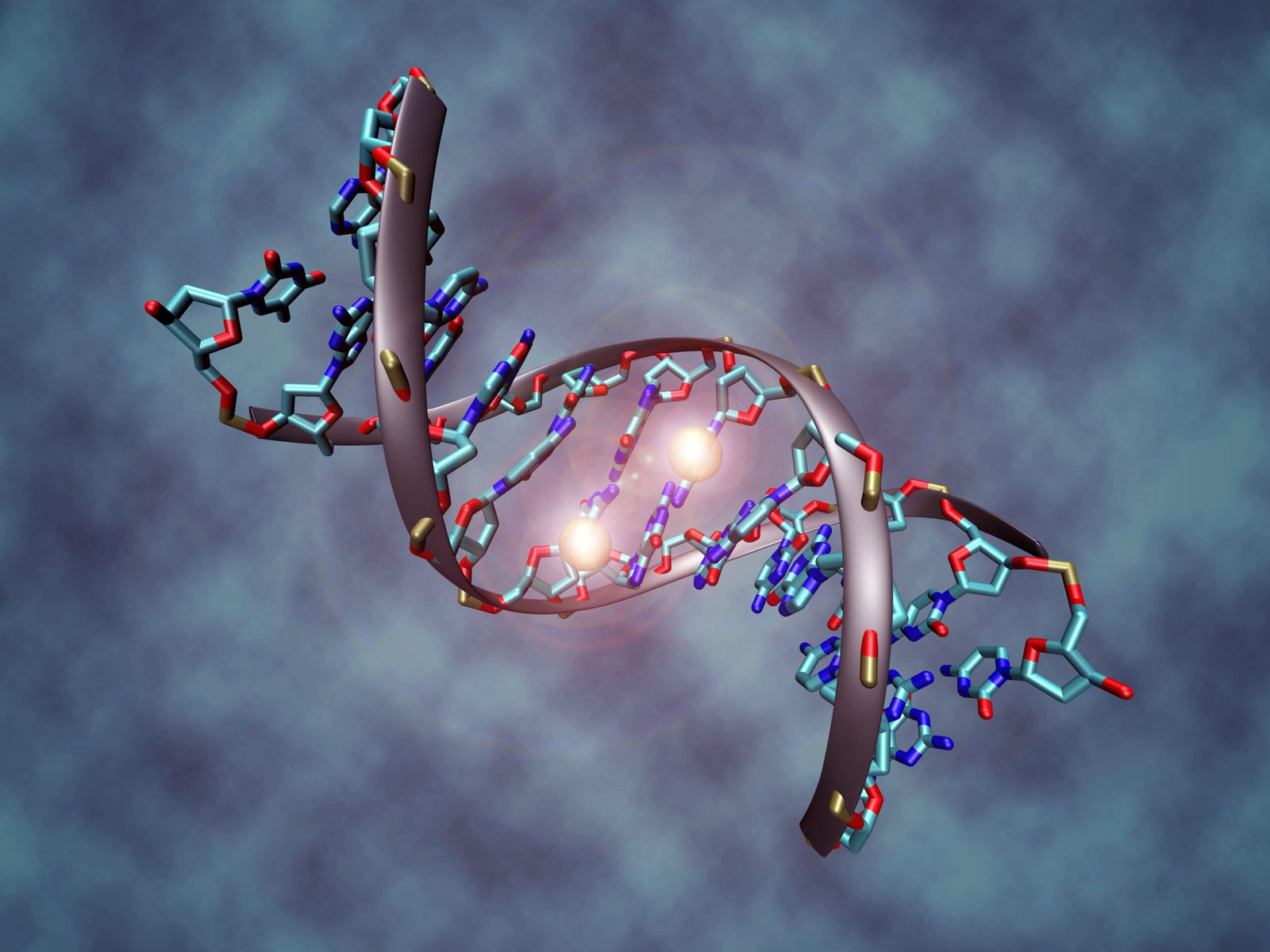
Chronic stress doesn’t usually mutate DNA, but it changes what the genome chooses to say. Chemical tags on DNA and histones adjust the volume of hundreds of genes, sometimes for months or years. It’s a survival notebook: prioritize rapid fuel, dampen long-term growth, keep immune troops ready. That notebook can help in hard seasons, but it can also trap biology in yesterday’s weather. Children and caregivers exposed to prolonged strain, for instance, often show stress-tilted gene regulation well beyond the event.
These epigenetic edits are not destiny, yet they’re not easily erased either. Lifestyle shifts, therapy, and targeted drugs can nudge the marks back, like sanding grooves out of wood. The science is marching toward precision: identify which marks predict which outcomes, then intervene early. Imagine routine panels that track stress-related methylation the way cholesterol is checked today. Prevention could move upstream, where biology first bends.
Energy, Inflammation, and the Cellular Battlefield
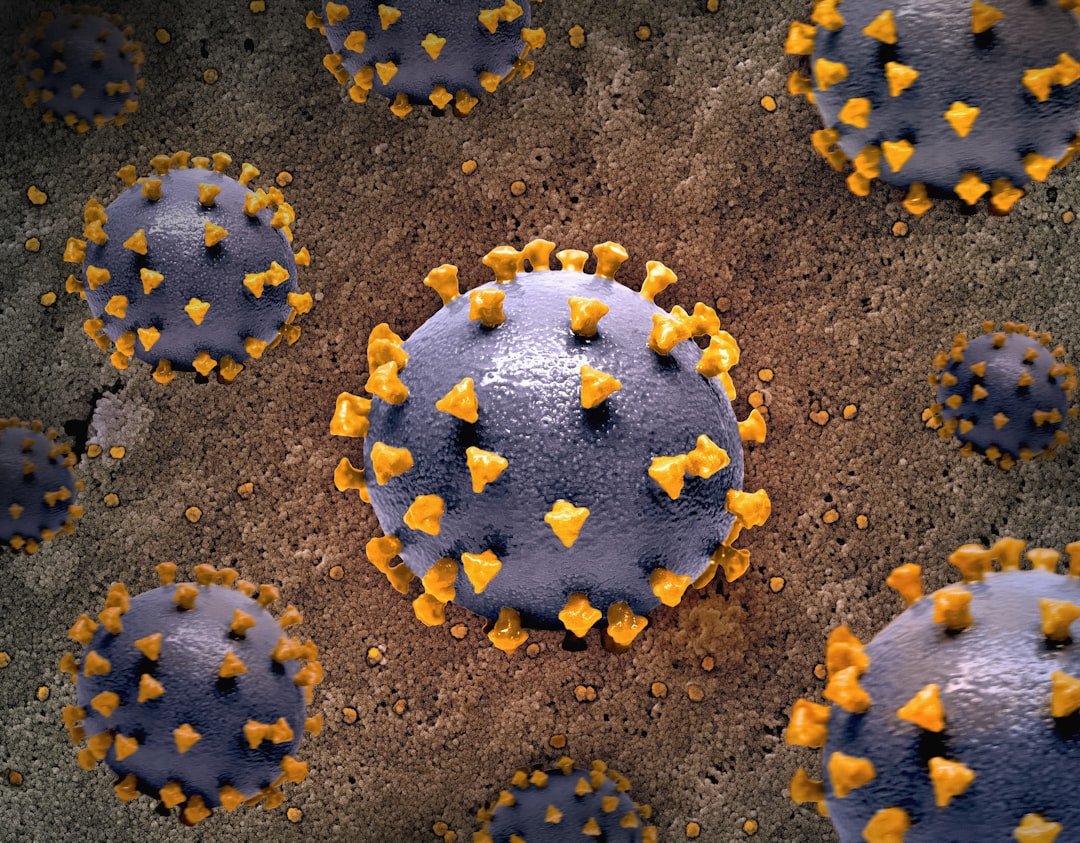
Stress reroutes energy, pushing cells to burn quick fuels and accept more oxidative sparks from mitochondria. That trade-off is like sprinting with a backpack: you move fast, but the straps chafe and the load grows heavier. Reactive molecules nick proteins and lipids, while repair crews fall behind. Inflammasomes ignite, calling immune squads that sometimes overshoot the target. Tissue becomes a battlefield with friendly fire.
Meanwhile, immune cells themselves change character under chronic stress, favoring short-term defense over nuanced regulation. Infections may linger longer, vaccines may work a bit less reliably, and healing can stall at the halfway mark. Fat cells whisper inflammatory cues into the bloodstream, stitching stress to metabolic disease. In the brain, microglia prune connections more aggressively, reshaping circuits linked to mood and memory. Biology is not broken, just stuck in siege mode.
Why It Matters
For decades, stress was treated as a feeling to be managed rather than a biology to be measured. We told people to relax; we rarely checked what their cells were doing. That’s changing, and the shift mirrors cardiology’s transformation from “chest pain” to precise biomarkers and imaging. When medicine treats stress as a cellular state, prevention looks different, screening looks different, and treatment becomes more targeted. The payoff could be fewer heart attacks, calmer autoimmune flares, and better outcomes in depression and anxiety.
This also reframes responsibility. Stress isn’t just a personal failing or a time-management glitch; it’s influenced by work schedules, housing, discrimination, and climate shocks. Comparing individuals without accounting for those forces misses the real levers. Policy and workplace design become part of the prescription, alongside therapy and medication. If we measure what matters, we’ll finally fund what works.
The Future Landscape

The next wave combines wearables, lab-on-a-chip chemistry, and machine learning to track stress in context. Noninvasive sensors for cortisol and related metabolites are advancing, while smart rings and watches capture sleep depth, heart-rate patterns, and temperature drift. Link those streams to single-cell signatures from blood spots, and you get a personalized stress map that updates like a weather app. Digital twins – computational stand-ins of your biology – could simulate how exercise, light exposure, or a new medication will shift your cellular state. Care plans might become truly adaptive, changing week by week instead of visit by visit.
But the road is bumpy. Privacy risks loom when stress fingerprints reveal mental health history or job burnout. Algorithms trained on narrow populations can misread signals in others, widening gaps in care. Clinical trials must prove that tracking these biomarkers actually improves outcomes, not just dashboards. The greatest challenge is humane design: tools that reduce stress rather than add another alert to ignore. If we get that right, prevention can finally outrun the problem.
Conclusion

Start with simple, measurable nudges that talk to your cells’ clocks and fuel lines. Keep a consistent sleep and wake window across the week, and get morning light to anchor circadian timing. Add a brief, daily practice of slow breathing or a short walk – microdoses of calm that lower the baseline alarm. Build a social safety net you can actually reach, even if it’s just one friend for a weekly check-in. And if stress is spilling into pain, sleep loss, or heavy mood, treat it like any medical concern and ask for care early.
At the community level, support workplaces that cap after-hours messaging, schools that protect recess and arts, and cities that invest in green spaces where biology can idle down. Back studies that test stress-biology interventions in diverse groups so they work for everyone. Advocate for insurance coverage that includes prevention, not only crisis response. I keep a sticky note on my desk that simply says: fewer alarms, clearer rhythms. What one rhythm will you protect this week?

Suhail Ahmed is a passionate digital professional and nature enthusiast with over 8 years of experience in content strategy, SEO, web development, and digital operations. Alongside his freelance journey, Suhail actively contributes to nature and wildlife platforms like Discover Wildlife, where he channels his curiosity for the planet into engaging, educational storytelling.
With a strong background in managing digital ecosystems — from ecommerce stores and WordPress websites to social media and automation — Suhail merges technical precision with creative insight. His content reflects a rare balance: SEO-friendly yet deeply human, data-informed yet emotionally resonant.
Driven by a love for discovery and storytelling, Suhail believes in using digital platforms to amplify causes that matter — especially those protecting Earth’s biodiversity and inspiring sustainable living. Whether he’s managing online projects or crafting wildlife content, his goal remains the same: to inform, inspire, and leave a positive digital footprint.