The battle between humans and viruses has raged for millennia, but what if we could flip the script entirely? Instead of treating viral infections after they occur, imagine having DNA that’s naturally programmed to resist virtually every virus known to science. This isn’t science fiction anymore – researchers are getting remarkably close to making this reality possible through groundbreaking genetic engineering techniques.
Think about it like this: your smartphone gets regular security updates to protect against new threats, but what if your body could have a similar built-in antiviral system? Scientists are now exploring ways to essentially “upgrade” human DNA to create universal resistance against viral pathogens. From CRISPR gene editing to engineered immune responses, the possibilities are both thrilling and complex. Let’s dive into this fascinating world where biology meets engineering to discover just how close we are to creating virus-resistant humans.
CRISPR Technology Leading the Antiviral Revolution
CRISPR genome editing has made remarkable strides in targeting viruses directly, with trials like those by Excision Biotherapeutics showing that guide RNAs can direct the Cas9 protein to cut at specific sites within viral genomes, surgically excising most of the viral DNA and effectively eliminating it from infected cells. The CRISPR-Cas9 system can be engineered to introduce site-specific breaks within viral genomes like Hepatitis B Virus, disrupting essential viral genes and inhibiting viral replication.
Scientists have developed innovative approaches using bacteriophages engineered to contain CRISPR-Cas3 systems, where the Cas3 protein shreds DNA at targeted gene regions, specifically targeting the genomes of bacterial pathogens. This represents a fundamental shift from traditional antiviral approaches to precision-guided genetic interventions. The technology works by programming cells to recognize and destroy specific viral sequences before they can establish infections.
Universal Antiviral Protection Through Genetic Engineering

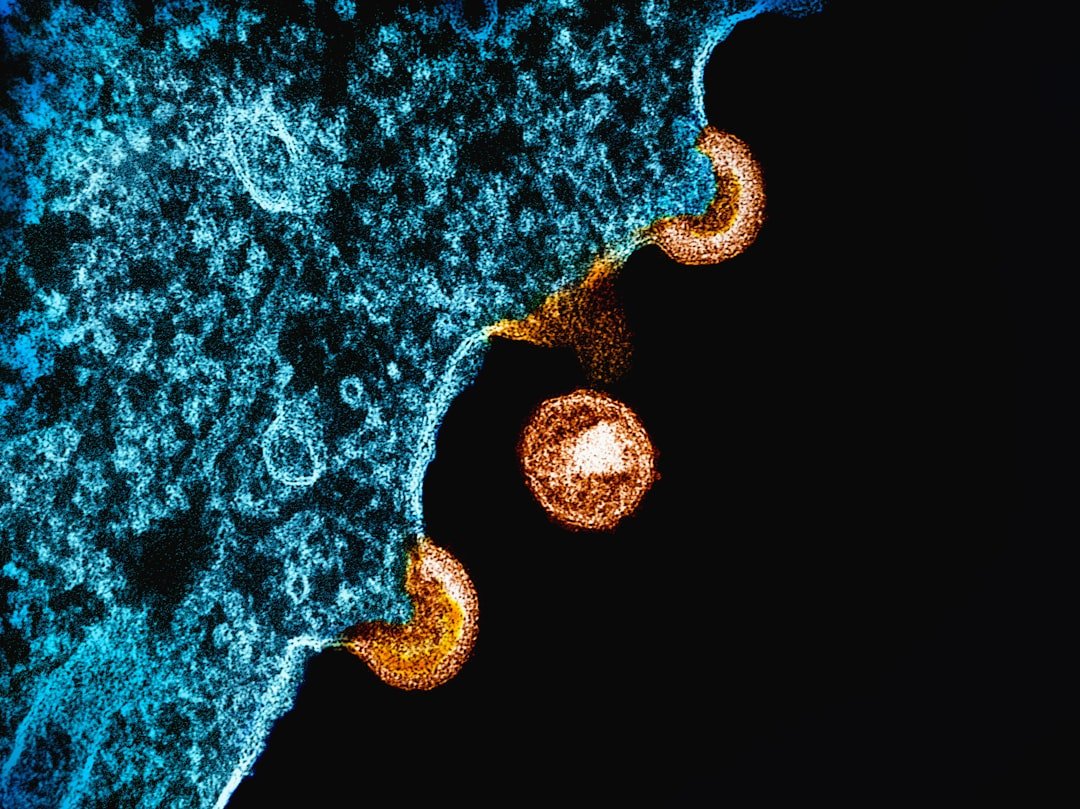
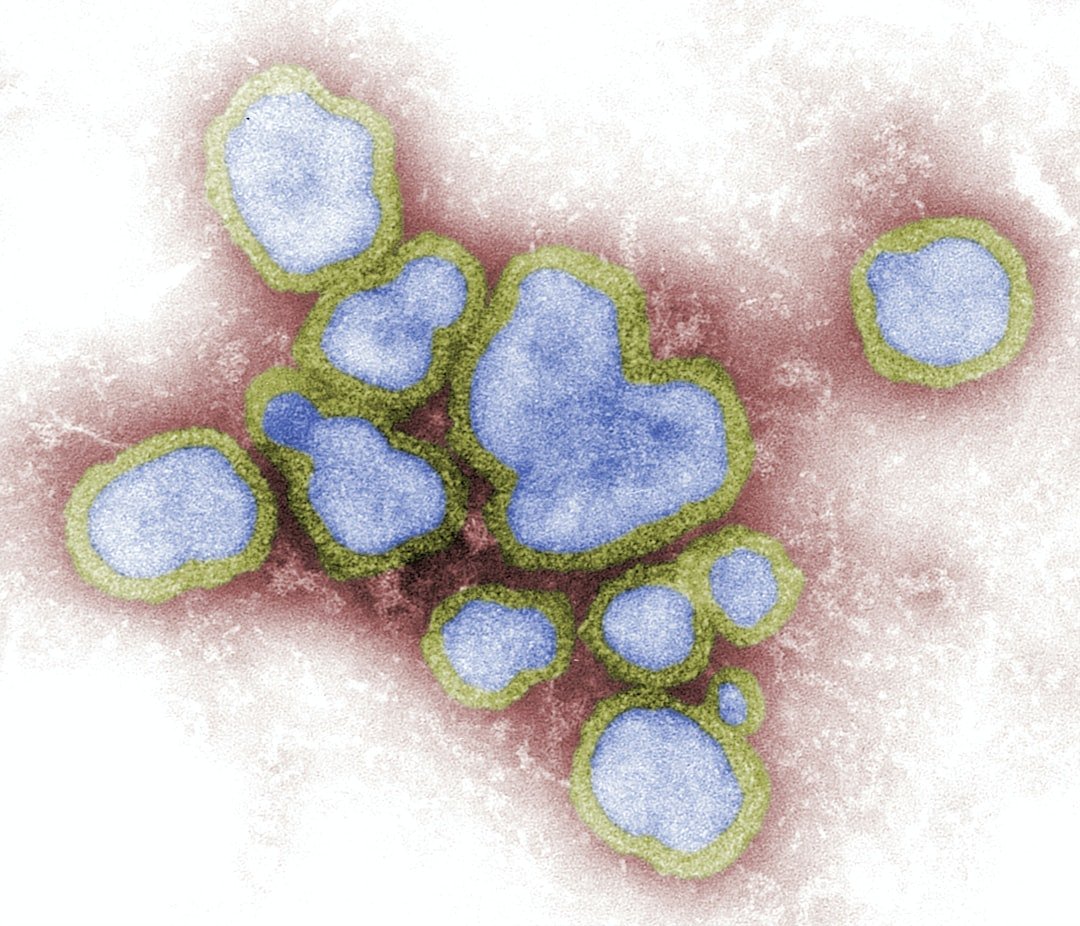
Recent breakthrough research published in Science Translational Medicine demonstrates how experimental therapies inspired by immune system studies aim to provide broad antiviral protection, potentially preventing viral replication of influenza and SARS-CoV-2 viruses when administered prophylactically, with researchers reporting they have yet to find a virus that can break through the therapy’s defenses in cell culture.
Instead of targeting individual viruses, this approach turns on production of ten specific proteins that provide broad antiviral protection, using a design similar to COVID mRNA vaccines but packaging ten mRNAs encoding these proteins inside lipid nanoparticles, allowing recipient cells to generate the antiviral proteins with only minimal inflammation needed to prevent viral diseases. This represents a paradigm shift toward universal protection rather than virus-specific treatments.
The Natural Immunity Blueprint Scientists Are Copying
The inspiration for universal antiviral protection comes from individuals with ISG15 deficiency, a rare genetic condition that typically increases susceptibility to severe viral infections, particularly mycobacterial infections and influenza through persistent systemic inflammation that encounters all sorts of viruses including flu, measles, mumps, and chickenpox.
Research on ISG15 deficiency has provided insights into antiviral immunity mechanisms, though individuals with this condition typically face increased viral susceptibility, because the usual brakes on the immune system’s antiviral machinery never fully engage, leaving certain virus-fighting proteins active all the time. This natural experiment in human genetics provides the roadmap for engineering similar protection in everyone else.
Engineering Bacteria as Living Antiviral Factories
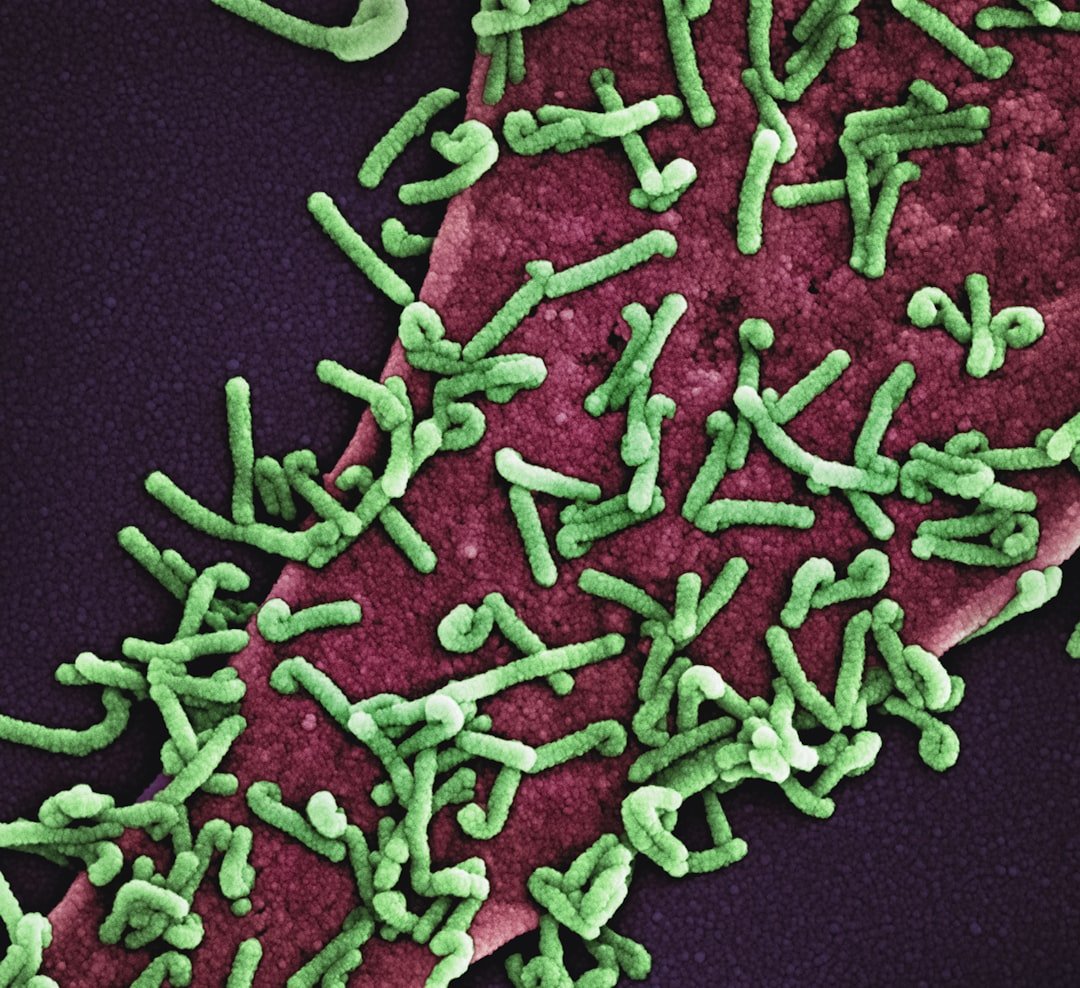
Scientists have developed engineered probiotic platforms using bacteria like Escherichia coli Nissle 1917, capable of providing both mucosal and systemic immunity through oral administration by displaying anti-spike nanobodies or expressing viral proteins on the bacterial surface, effectively inhibiting virus-receptor interactions and facilitating the translocation of therapeutic molecules to distant organs through outer membrane vesicles.
These engineered bacteria keep their therapeutic cargo displayed on the bacterial surface and harness outer-membrane vesicles as nano-sized delivery vehicles that naturally shed from bacteria, traffic through the gut epithelium, enter blood circulation and distribute their antiviral payload to distant tissues. This approach creates living, self-replicating antiviral factories that can be administered as simply as taking a probiotic supplement.
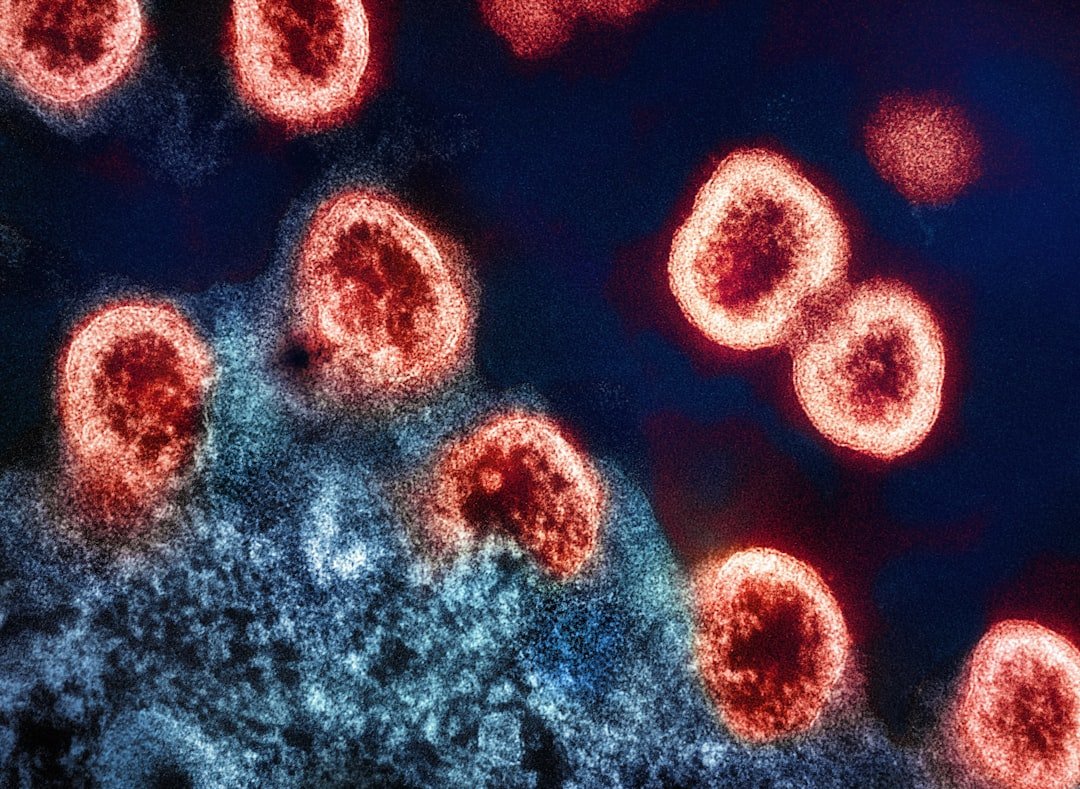
Targeting Viral DNA Integration and Persistence
Engineered endonucleases including homing endonucleases, zinc finger nucleases, CRISPR/Cas9 and other systems can target specific DNA sequences for cleavage and are proving valuable as therapeutics for treating infectious pathogens, with recent efforts focusing on using these gene-editing platforms as antiviral therapeutics. These approaches specifically target latently integrated or nonreplicating episomal viral genomes that traditional therapies cannot eliminate, using endonucleases engineered with high specificity to minimize off-target binding while repeatedly cleaving critical sites to permanently disrupt translation of essential viral proteins.
The strategy represents a curative rather than suppressive approach to viral infections. By cutting out viral DNA that has integrated into host cells, scientists can potentially eliminate persistent infections like HIV, hepatitis B, and herpes simplex virus that current drugs can only manage but not cure.
Advanced Delivery Systems and Precision Targeting
Researchers have adapted COVID-19 vaccine technology, using modified messenger RNA packaged in lipid nanoparticles, but instead of carrying instructions for viral spike proteins, these particles deliver genetic blueprints for ten specific antiviral proteins that have shown effectiveness against a broad range of viruses in laboratory tests. However, drug delivery and absorption properties still need optimization, as current delivery methods produce proteins in target tissues but probably not at high enough levels for immediate human application, with the biggest challenge being delivery of nucleic acids to the specific body parts requiring protection.
The precision required for these systems is extraordinary. Think of it like trying to deliver a software update to every smartphone in a city, but each phone needs a different update and you have to make sure the right update reaches the right device without interfering with normal phone functions.
Plant and Agricultural Models for Antiviral Engineering

Scientists have successfully used CRISPR technologies to directly target and interfere with pathogen genomes without affecting plant genomes, using DNA-targeting CRISPR systems like Cas9 to interfere with DNA viruses and RNA-targeting systems like Cas13 to disrupt RNA genomes or RNA transcripts of pathogens. The use of CRISPR in agriculture is becoming increasingly common worldwide, with researchers adapting CRISPR tools for new species and purposes, from reducing waste to adapting organisms to climate change, demonstrating the versatility of gene editing for pathogen resistance.
These agricultural applications serve as proof-of-concept for human applications. Plants engineered with CRISPR show that it’s possible to create organisms with broad-spectrum pathogen resistance while maintaining normal biological functions.
Overcoming Off-Target Effects and Safety Challenges

A key concern that poses severe limitations in clinical applications is off-target effects, where unintended CRISPR editing can result in mutations and genomic instability that may put patients’ lives at risk. Scientists have addressed this by developing enhanced SpCas9 variants like eSpCas9, SpCas9-HF1, and hypaCas9 that demonstrate higher on-target activity and significantly lower off-target effects through rational protein engineering and proof-reading mechanisms that trap these mutants in inactive states when bound to mismatched targets.
Powerful strategies to minimize off-target editing include engineering Cas9 variants with improved target specificity, including high-fidelity Cas9 enzymes that are more effective at discriminating against mismatches, with researchers able to assess and mitigate risks of unintended mutations during the research and development phase. The safety improvements are dramatic – some newer systems show nearly complete elimination of off-target effects.
Challenges of Viral Evolution and Resistance
A major challenge is that genetic mutations could destroy enzyme recognition sites while leaving functional viral proteins intact, creating latently infected cells immune to further enzyme activity, similar to how viruses develop resistance to antiviral agents, requiring concurrent use of multiple targeting approaches just as HIV treatment uses multiple drugs to minimize resistance. Rapidly evolving viruses like influenza, HIV, and Ebola routinely circumvent therapeutic intervention through mutational escape, with error-prone genome replication generating heterogeneous viral populations that rapidly adapt to new selection pressures.
The three core challenges in antiviral therapy are resistance (viruses mutate while pharmaceuticals do not), persistence (viruses evolved to remain in hosts while pharmaceuticals are cleared), and transmission (viruses are communicable while pharmaceuticals are not), creating fundamental mismatches between viral characteristics and current intervention approaches. This evolutionary arms race means that any engineered resistance must be designed to adapt alongside viral mutations.
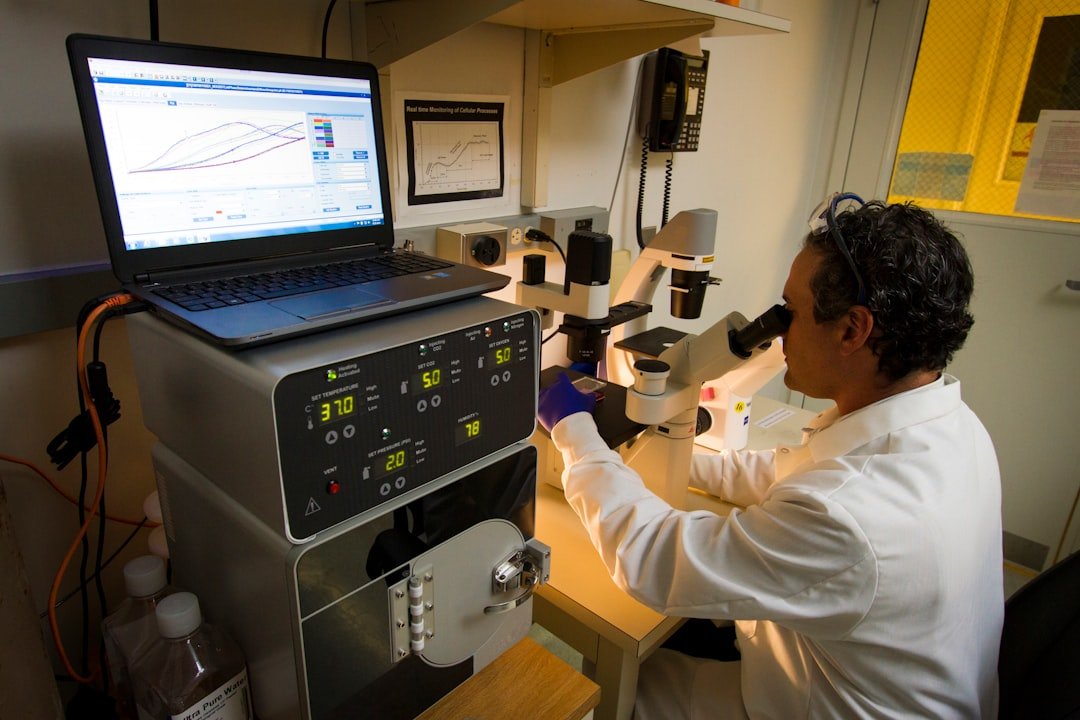
Current Clinical Progress and Future Applications
Recent clinical trials represent the first to target chronic viral infections using CRISPR-based approaches. Researchers envision this technology as a weapon for the next pandemic, providing protection for first responders, nursing home residents, and family members of infected individuals, regardless of the specific virus responsible. If technical challenges around delivery are solved, the next pandemic might be met not just with lockdowns and masks, but with nasal sprays that provide immune systems with universal viral shields, representing the potential development of a truly universal antiviral for everyone.
The timeline for human applications remains uncertain, but the rapid progress in both laboratory research and early clinical trials suggests we may see limited applications within the next decade. The most promising near-term applications will likely focus on protecting high-risk populations during disease outbreaks rather than providing universal resistance to healthy individuals.
Conclusion: The Promise and Reality of Universal Viral Resistance
The dream of engineering DNA to resist all viruses is no longer purely theoretical. Scientists have demonstrated remarkable progress in multiple approaches, from CRISPR-based viral genome disruption to engineered bacteria that act as living antiviral factories. The discovery that some humans naturally possess near-universal viral resistance has provided a biological blueprint that researchers are now working to replicate through various technological approaches.
However, significant challenges remain. Delivery systems need improvement, off-target effects require continued refinement, and the evolutionary nature of viruses means that any engineered resistance must be adaptable. The complexity of creating truly universal viral resistance – protection against both known and unknown pathogens – represents one of the most ambitious goals in modern medicine. While we may not achieve complete viral immunity in the immediate future, the foundations being laid today could transform how humanity responds to viral threats in the coming decades. What once seemed impossible is now merely extraordinarily difficult.