An HIV diagnosis was thought of as a death sentence for decades. Millions of people living with the virus lead long, healthy lives today thanks to revolutionary medical advances. One still unresolved issue is whether HIV/AIDS can ever be totally cured. The response is more hopeful and complicated than you would think.
Although ART can lower HIV to undetectable levels, completely eradicating the virus has proved far more difficult. Under unusual conditions, only a small number of people have been cured; hence, scientists are racing to discover the keys of a long-term fix. From stem cell transplants to innovative gene-editing technologies, HIV treatment’s future promises both possibilities and unresolved questions.
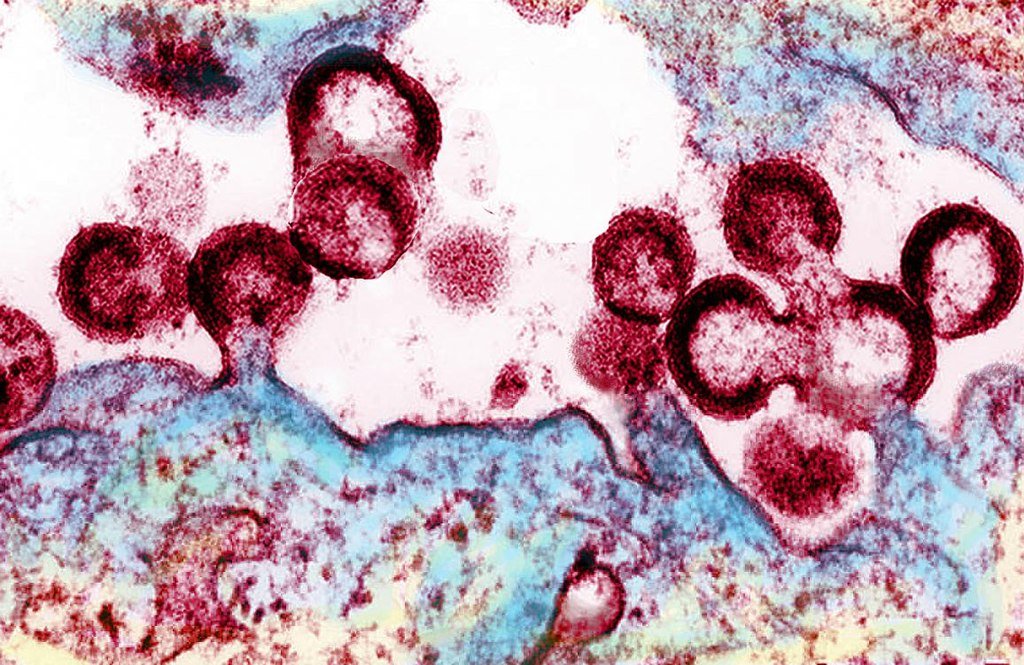
How HIV Hijacks the Immune System
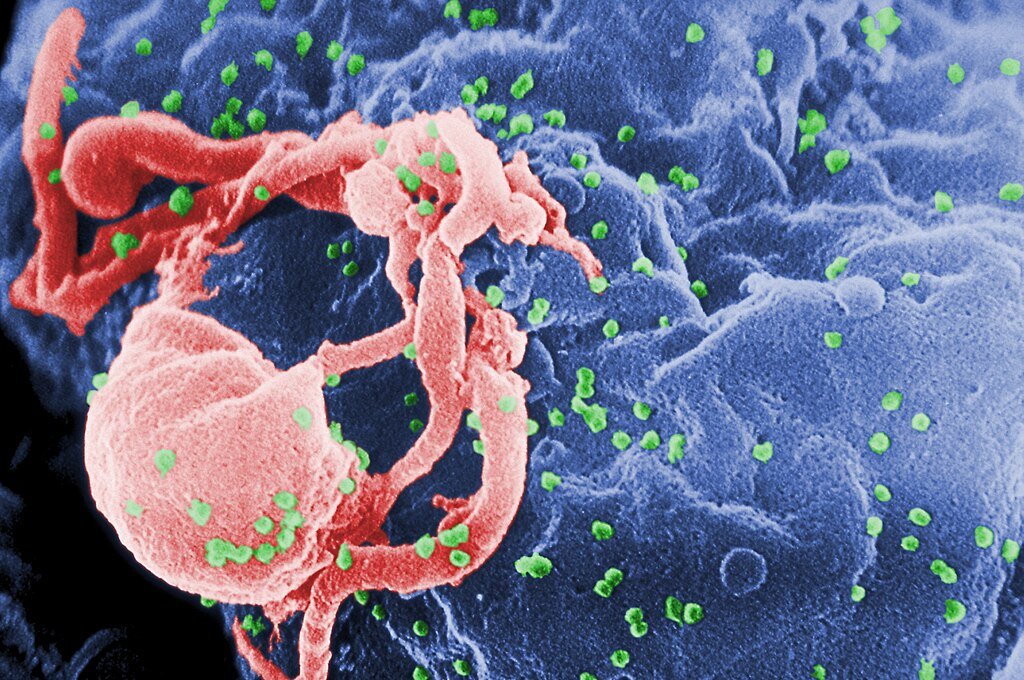
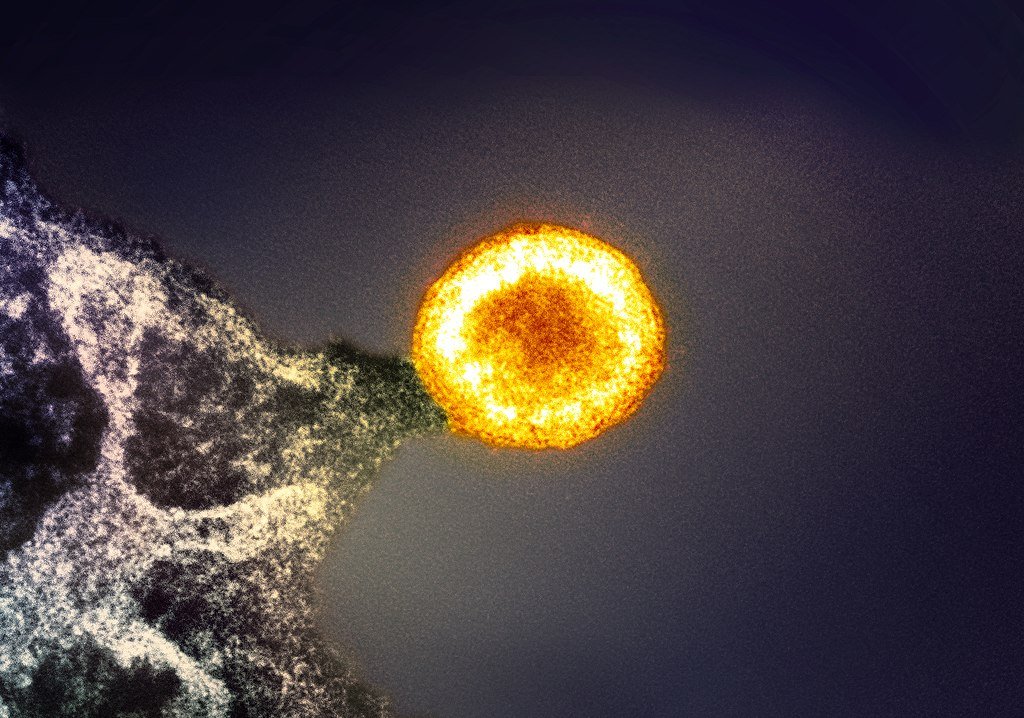
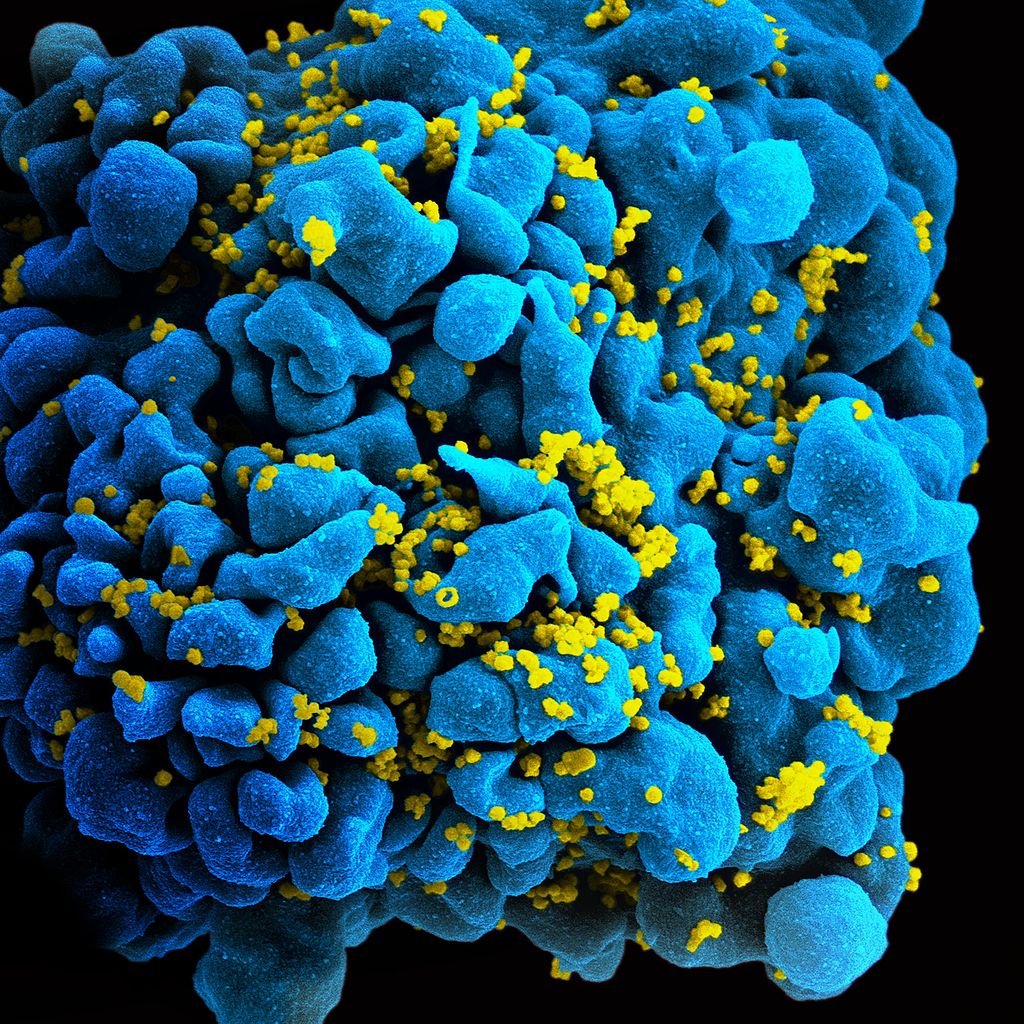
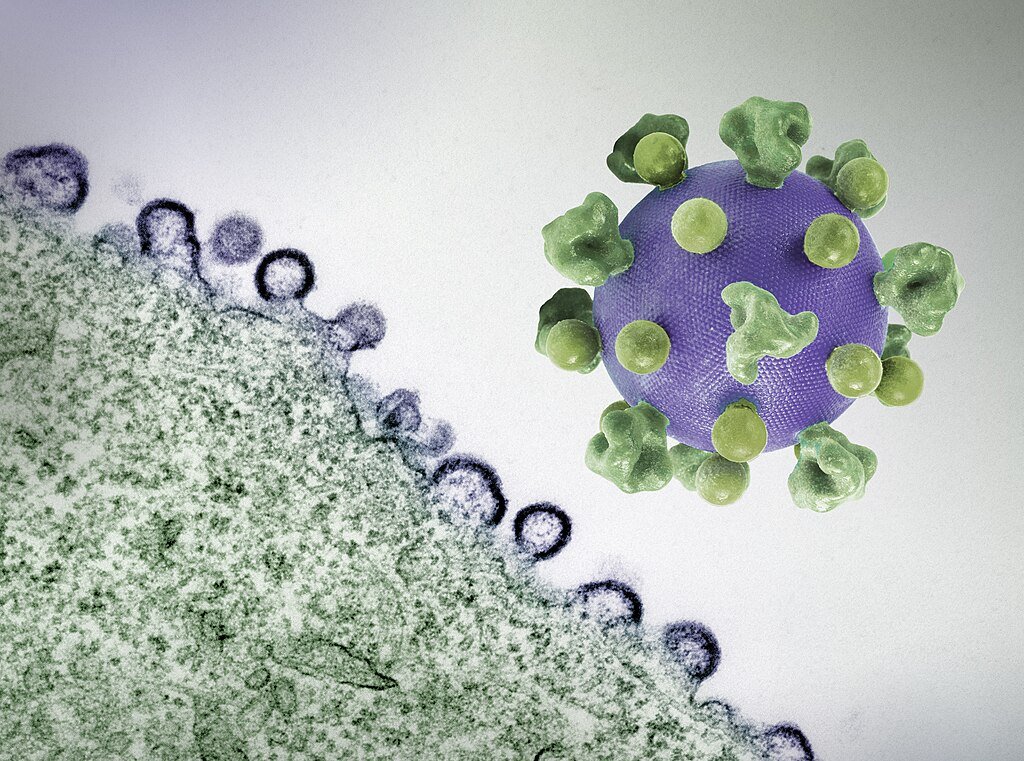
HIV (human immunodeficiency virus) particularly targets CD4 T-cells, the front-line immune system defenders. This is a retrovirus. Once inside, the virus uses the DNA of the host cell and its genetic code to build a factory for HIV production. This ongoing reproduction over time runs down CD4 cells, so compromising the body’s ability to fight infections.
HIV progresses to acquired immunodeficiency syndrome without treatment, in which case even minor infections can be fatal since the immune system is so weakened. Usually taking 8–10 years, ART may cause a delay always. Notwithstanding this, 39.9 million people globally will have HIV in 2023 and 630,000 deaths from AIDS-related diseases show that availability to treatment still poses a significant challenge.
The Elusive Cure: Why HIV Is So Hard to Eradicate
Unlike most viruses, HIV hides itself in long-lived memory cells of the body, so avoiding immune detection and conventional treatments. Should treatment stop, these dormant cells can reactivate even if ART lowers viral load to “undetectable” levels.
Out of all the high-risk stem cell transplants meant to treat blood cancers, only five persons have been verified as HIV cured. Using rare CCR5-delta32 mutant donor cells, these transplants prevent HIV from entering CD4 cells. The most well-known example, Timothy Ray Brown’s “Berlin Patient,” stayed HIV-free until his 2020 cancer death.
Stem cell transplants are dangerous, costly, and unworkable for most patients, thus these treatments come at a heavy price. To copy these findings without the great risks, researchers are now looking at safer substitutes including immune-boosting medications and gene therapy.
Undetectable = Untransmittable: How Treatment Prevents Spread
Although most people still live far from a cure, ART has transformed HIV treatment. Taken regularly, these medications so powerfully suppress the virus that those with undetectable viral loads cannot spread HIV sexually, a breakthrough known as “U=U” undetectable = untransmittable.
- Reduced transmission risk comes from viral suppression of fewer than 200 copies/mL of blood.
- When taken as directed, pre-exposure prophylactic treatment (PrEP) tablets lower infection risk by 99%.
- On ART, pregnant women can reduce the transmission to their unborn children to under 1%.
Still, 20% of HIV-positive people worldwide lack access to treatment, which fuels ongoing new infections. The epidemic cannot be stopped without closing this disparity.
The Future of HIV Cure Research
Scientists are pursuing multiple strategies to cure HIV, including:
1. “Shock and Kill” Therapy
This strategy uses drugs that activate the virus to flush out latent HIV from reservoirs, destroying the exposed cells. Early studies show promise but find difficulty focusing just on infected cells.
2. Gene Editing (CRISPR)
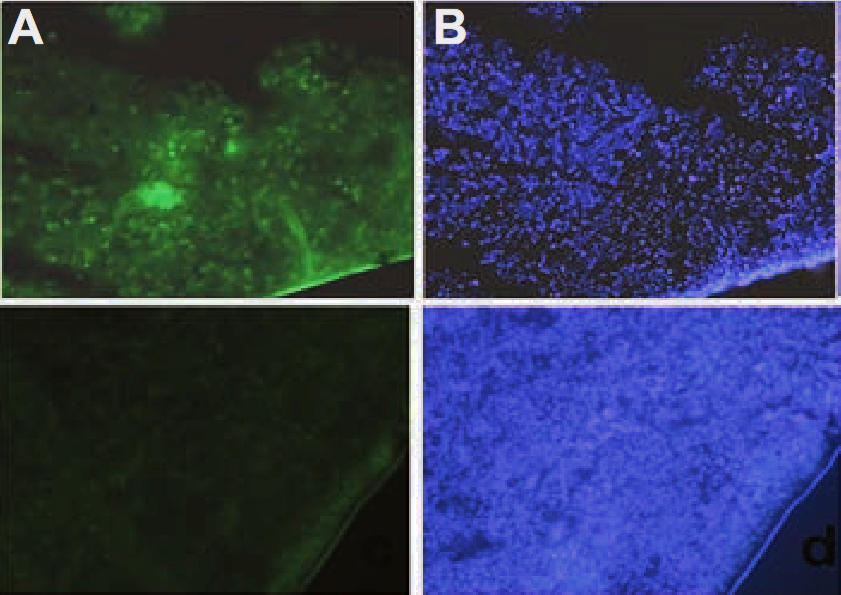
Either cutting HIV DNA out of infected cells or altering immune cells to fight infection, Crispen technology could be a big first towards human trials, researchers effectively eliminated HIV from mice using CRISpen in 2022.
3. Immune-Based Therapies
Some “elite controllers” suppress HIV naturally without medication. Researchers are looking at their immune reactions to create antibody treatments or vaccinations having a similar impact.
4. Long-Acting Injectables
Daily tablets could be replaced by new monthly or annual injectable ART, so improving adherence and lowering stigma.
Conclusion: Hope, But No Easy Answer
Since a real cure is rare and experimental, HIV is no longer the death sentence it once was. Right now, the best weapons for virus control are prevention, early testing, and consistent treatment.
Whether by gene editing, immunological treatments, or other unanticipated discovery, the next decade could bring innovations. Science keeps relentlessly seeking a world in which HIV is not only treatable but also manageable until then.
One thing is definite: the battle is far from finished.
Source:

Suhail Ahmed is a passionate digital professional and nature enthusiast with over 8 years of experience in content strategy, SEO, web development, and digital operations. Alongside his freelance journey, Suhail actively contributes to nature and wildlife platforms like Discover Wildlife, where he channels his curiosity for the planet into engaging, educational storytelling.
With a strong background in managing digital ecosystems — from ecommerce stores and WordPress websites to social media and automation — Suhail merges technical precision with creative insight. His content reflects a rare balance: SEO-friendly yet deeply human, data-informed yet emotionally resonant.
Driven by a love for discovery and storytelling, Suhail believes in using digital platforms to amplify causes that matter — especially those protecting Earth’s biodiversity and inspiring sustainable living. Whether he’s managing online projects or crafting wildlife content, his goal remains the same: to inform, inspire, and leave a positive digital footprint.