Imagine if every autumn, you needed a brand-new shield to protect yourself from a sneaky, ever-changing enemy. That’s the reality for everyone who faces flu season each year. The flu shot you get this year isn’t the same as last year’s—and next year’s will be different, too. Why? Because influenza is a master of disguise, constantly reinventing itself and keeping even the world’s best scientists on their toes. The science behind the annual flu vaccine is a story of global detective work, high-stakes prediction, and a race against time. Let’s pull back the curtain on why the flu shot changes every year and explore the fascinating—and sometimes frustrating—science of viral guesswork.
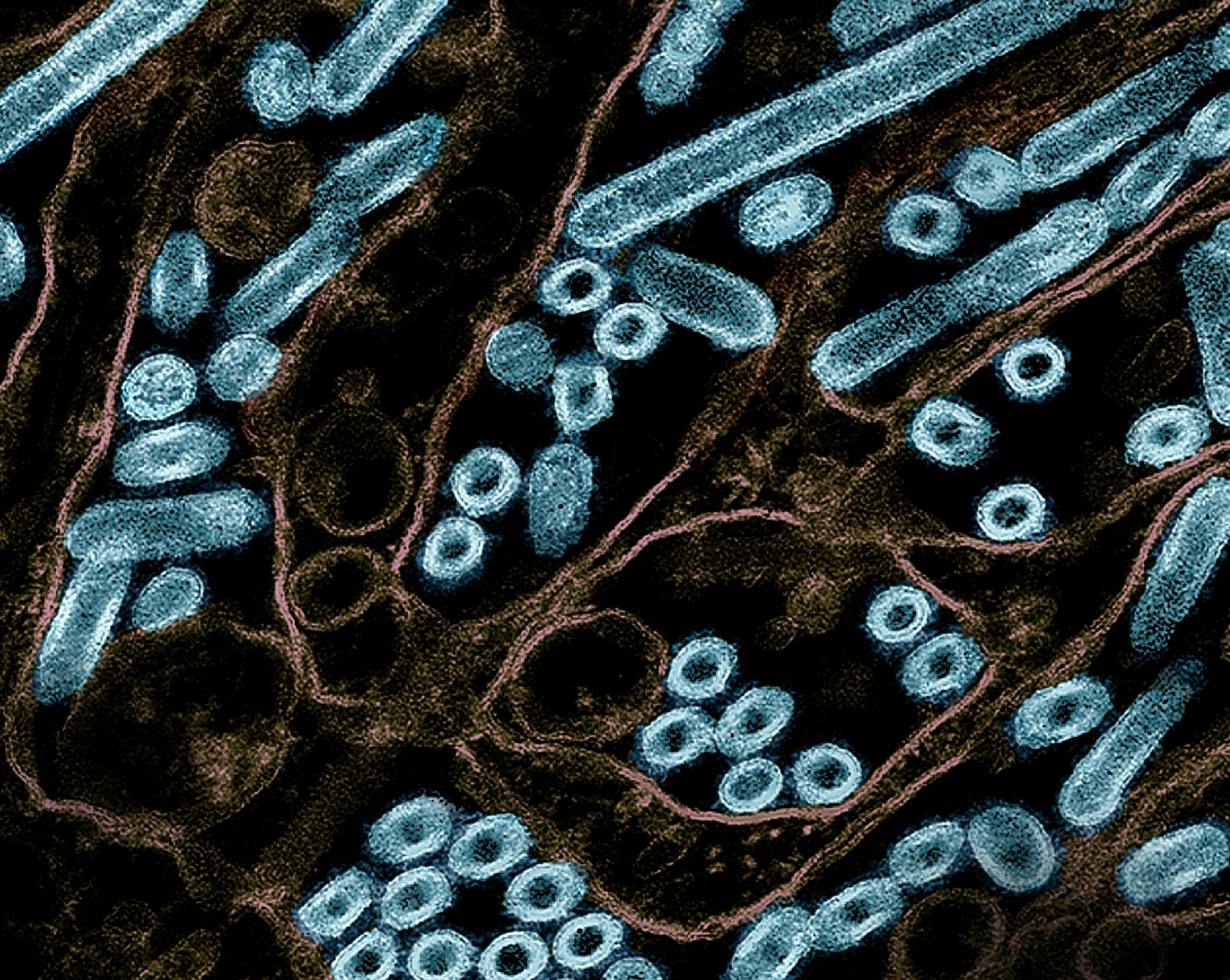
The Shape-Shifting Nature of Influenza Viruses
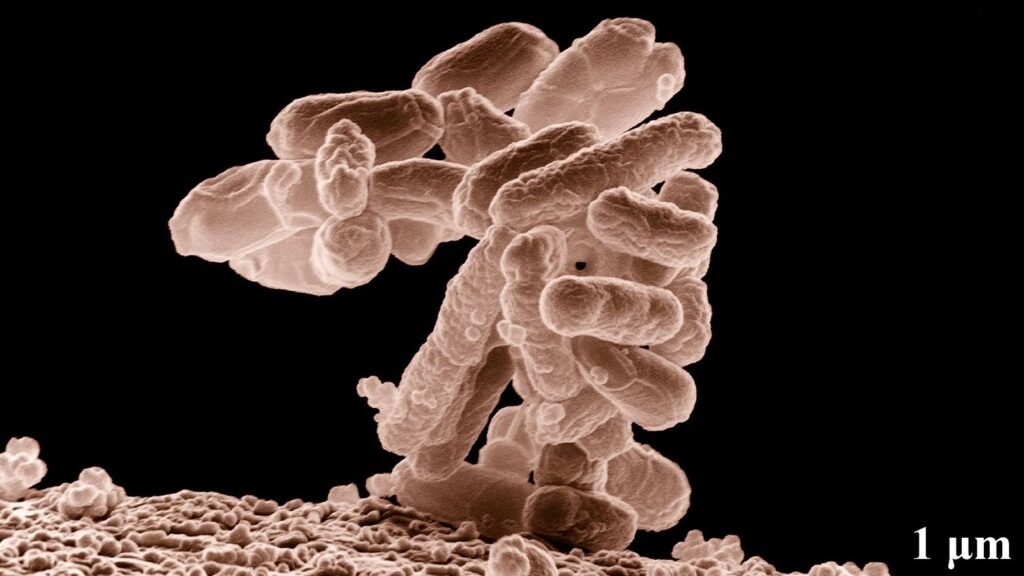
Influenza viruses are notorious for their ability to mutate at lightning speed. Unlike many viruses, the flu’s genetic code is built from RNA, which is far more prone to errors during reproduction than the DNA found in humans. These errors, or mutations, create endless new viral versions, each with slightly different surface proteins. Think of the flu as a master chef constantly tweaking the recipe, adding new ingredients, and changing the flavor, making it hard for our immune system to recognize and fight it. This constant change is why last year’s vaccine can quickly become outdated, leaving scientists in a perpetual game of catch-up.
What’s in a Name? Understanding Flu Virus Types and Subtypes
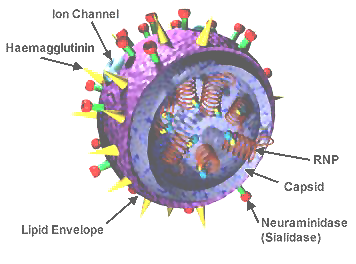
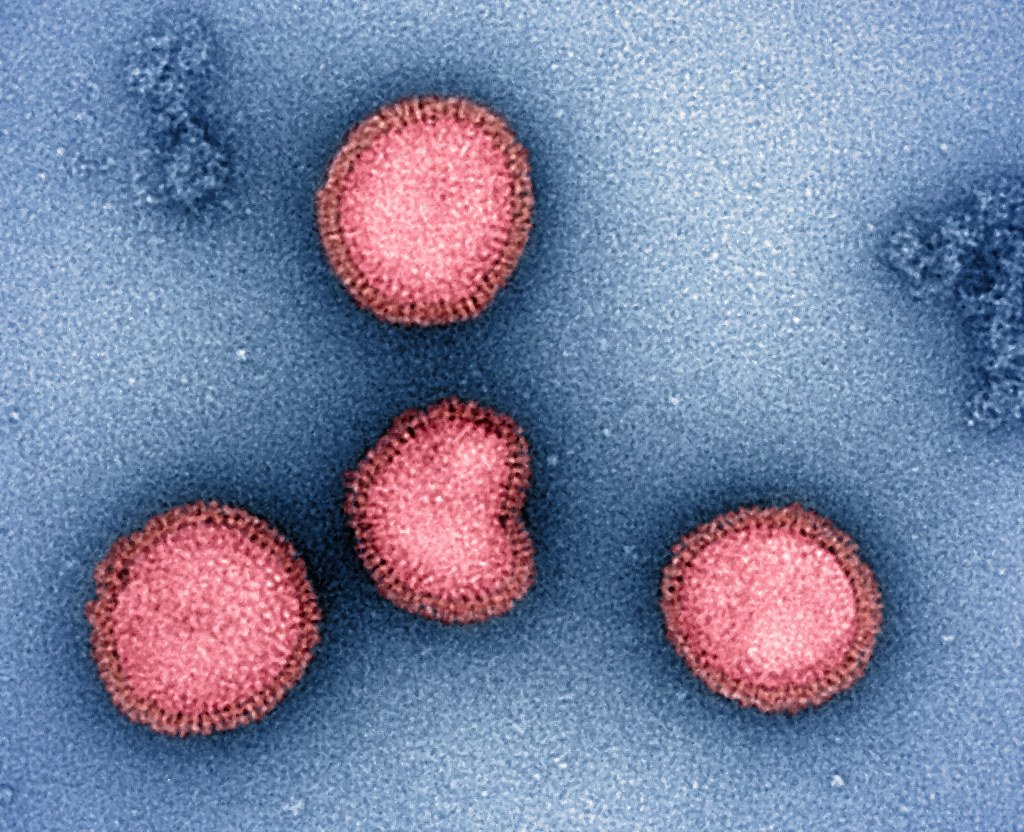
There’s not just one “flu”—there are actually several types, with influenza A and B being the most common culprits in seasonal outbreaks. Influenza A is especially tricky because it comes in many subtypes, identified by two proteins: hemagglutinin (H) and neuraminidase (N). You might have heard of H1N1 or H3N2, for example. Each combination can trigger a unique outbreak. Influenza B has its own lineages, like Victoria and Yamagata, which also change over time. This variety is like a vast wardrobe of costumes, allowing the virus to keep fooling immune systems year after year.
Antigenic Drift: The Slow Creep of Change
One of the main reasons the flu shot needs updating is antigenic drift. This is the gradual, small-scale mutation of the virus’s surface proteins, especially hemagglutinin and neuraminidase. Over time, these changes add up, leading to significant differences from older versions. Imagine a game of telephone where the message is whispered from person to person—eventually, it’s nothing like the original. Even if you had the flu (or the vaccine) last year, your immunity may not recognize this year’s slightly altered virus, making you vulnerable all over again.
Antigenic Shift: The Sudden Leap
While antigenic drift is slow and steady, antigenic shift is a dramatic leap. This happens when two different flu viruses infect the same cell and swap genetic material, creating a brand-new subtype. It’s like two chefs combining recipes to invent an entirely new dish no one’s tasted before. Antigenic shift can lead to pandemics, as happened with the infamous 2009 H1N1 “swine flu.” Because these new strains are so different, few people have any natural immunity, making global outbreaks much more likely.
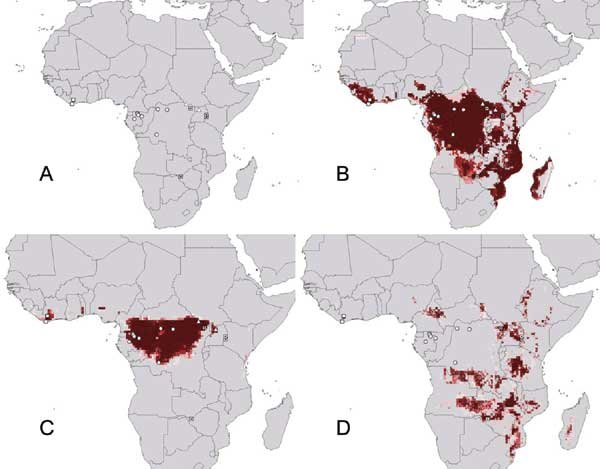
Chasing the Virus: Global Flu Surveillance
Around the world, scientists and health organizations are constantly hunting for clues about which flu strains are spreading. The World Health Organization (WHO) coordinates a global network of labs that collect samples from sick patients, analyze the viruses, and share their findings. Imagine a massive, international game of hide-and-seek with the virus always trying to stay one step ahead. This real-time surveillance is crucial for predicting which strains will dominate the upcoming flu season, but it’s far from foolproof.
The Art and Science of Viral Prediction
Every year, in February for the Northern Hemisphere and September for the Southern Hemisphere, experts gather to review the latest surveillance data. They examine which strains are spreading, how fast they’re mutating, and which ones seem poised to take over. It’s a bit like meteorologists trying to forecast the weather—there’s science, statistics, and a little bit of gut instinct. Based on their best judgment, they recommend which strains should go into the next season’s vaccine, hoping their predictions hit the mark.
The Time Crunch: Why Vaccines Must Be Made Months in Advance

Manufacturing flu vaccines isn’t quick or simple. Once the strains are chosen, companies need several months to produce, test, package, and distribute millions of doses worldwide. Most vaccines are still made using chicken eggs, a process that’s surprisingly delicate and time-consuming. That means decisions about which strains to include must be made long before the flu season actually begins—sometimes six months ahead. If the virus changes a lot during that time, the vaccine might not match the circulating strains, reducing its effectiveness.
Egg-Based Production: The Old-School Method

Most flu vaccines are still produced using a method developed in the 1940s: growing viruses in fertilized chicken eggs. The process starts by injecting the virus into the eggs, allowing it to multiply for several days, then harvesting and purifying it before adding it to vaccines. While this method is reliable, it’s slow and has some quirks. For example, the virus can mutate to adapt to the egg environment, sometimes making the resulting vaccine less effective. Newer methods using cell cultures or recombinant DNA are in development, but eggs remain the workhorse for now.
Why Vaccine Effectiveness Varies Year to Year
You might hear people grumble that the flu shot “didn’t work” one year. The truth is, effectiveness depends on how well the vaccine strains match the viruses actually circulating. Some years, scientists get it almost exactly right, and the vaccine provides strong protection. Other years, the virus drifts or shifts unexpectedly after the vaccine recipe is set, leading to a mismatch. Even in off years, though, the vaccine can still reduce the severity of illness, prevent complications, and save lives—especially among the most vulnerable.
Universal Flu Vaccine: The Holy Grail
Imagine a flu shot you get once, and you’re protected for years, even decades. That’s the dream behind the search for a universal flu vaccine—one that targets parts of the virus that rarely change. Researchers are exploring new targets, like the “stalk” of the hemagglutinin protein, which is more stable than the “head.” Progress has been slow, with some promising candidates in clinical trials as of 2025, but the finish line is still out of sight. If scientists succeed, it could transform flu prevention forever.
Real-World Impact: How the Flu Shot Saves Lives
Every year, the flu causes millions of illnesses, hundreds of thousands of hospitalizations, and tens of thousands of deaths worldwide. The annual vaccine isn’t perfect, but it’s the best defense we have. In years when the match is good, the shot can cut the risk of flu illness by up to 60%. It also helps protect people who can’t get vaccinated themselves—like infants or those with certain health conditions—by slowing down the virus’s spread. Getting the shot isn’t just about you; it’s about everyone around you, too.
Flu and COVID-19: A Complicated Dance
Since 2020, the world has watched as COVID-19 shook up everything, including flu season. Social distancing, mask-wearing, and lockdowns led to historic drops in flu cases, but now, as life returns to normal, flu is making a comeback. Scientists are studying how the two viruses interact, whether coinfections make people sicker, and how vaccine campaigns can adapt. Some researchers are even working on combination vaccines for flu and COVID-19, aiming for double protection in a single shot.
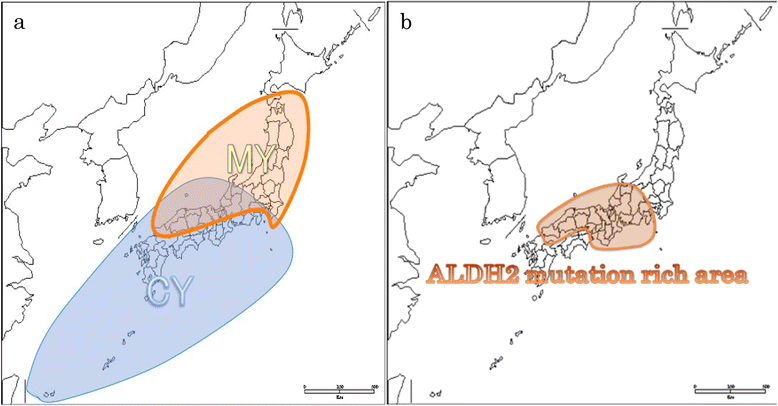
The Role of Animal Reservoirs in Flu Evolution
Flu viruses don’t just infect humans—they have a vast animal kingdom to call home. Birds, pigs, horses, and even dogs can carry their own flu strains. Sometimes, these viruses jump from animals to humans, a process called zoonosis. Pigs in particular are “mixing vessels,” where human and animal flu viruses can swap genes and create new strains. This animal reservoir is like a bubbling cauldron of genetic diversity, fueling the flu’s constant evolution and making prediction even harder.
Vaccination Fatigue: Overcoming Public Skepticism
After years of pandemic headlines, some people are weary of hearing about shots and vaccines. Flu vaccine uptake has dipped in certain groups, fueled by skepticism, misinformation, or simple apathy. Health officials face the challenge of communicating that, while the flu shot isn’t perfect, it’s still a critical tool for public health. Personal stories, clear messaging, and community outreach all play a part in encouraging people to roll up their sleeves each year.
The Economics of Flu Vaccines: Cost vs. Benefit
Producing and distributing flu vaccines is a massive undertaking, costing billions each year. But the return on investment is substantial: fewer hospitalizations, less time off work, and reduced pressure on healthcare systems. For every dollar spent on vaccination, studies suggest several dollars are saved in avoided medical costs. The annual campaign is an example of how science, policy, and economics intersect to protect society from a common—but potentially deadly—enemy.
Targeting the Most Vulnerable: High-Risk Groups
Flu is especially dangerous for certain groups: older adults, young children, pregnant women, and people with chronic illnesses. Vaccination campaigns prioritize these high-risk populations, offering special formulations like high-dose or adjuvanted vaccines for seniors. Protecting the most vulnerable isn’t just compassionate—it’s strategic. By reducing illness in those most likely to suffer complications, the overall burden of flu on society is reduced.
Innovation on the Horizon: mRNA and Beyond
The success of mRNA vaccines for COVID-19 has sparked new hope for flu prevention. mRNA technology allows for faster vaccine design, easier updates, and potentially stronger immune responses. Several companies are racing to develop and test mRNA-based flu vaccines, with early results looking promising. If these new vaccines succeed, the days of the slow, egg-based approach might finally come to an end, ushering in a new era of rapid, responsive flu protection.
Global Inequality in Vaccine Access
Not everyone has equal access to the annual flu shot. Wealthy countries typically have robust vaccination programs, while lower-income nations may struggle with supply, logistics, or costs. This global gap leaves millions at risk and allows flu viruses to circulate widely. Solving this challenge requires international cooperation, funding, and creative solutions to ensure everyone, everywhere, can benefit from the latest science.
The Human Side: Stories from the Front Lines

Behind every statistic are real people—nurses giving shots in crowded clinics, researchers working late to decode viral genomes, parents worrying for their children, and patients fighting for breath in hospital beds. The annual flu vaccine isn’t just a scientific achievement—it’s a testament to human resilience, ingenuity, and compassion. Every shot given is a small act of hope, a defiant stand against an ancient adversary that refuses to quit.
What You Can Do: Staying One Step Ahead
While the science of flu prediction will always involve some guesswork, you have the power to make a difference. Get your flu shot each year, encourage your friends and family to do the same, and stay informed about public health recommendations. Simple habits like handwashing, staying home when sick, and covering your cough can also help slow the spread. In the end, fighting the flu is a team effort, with each of us playing a vital role.
The next time you roll up your sleeve for a flu shot, remember the global detective work, high-speed evolution, and sheer human determination behind that tiny vial. Isn’t it wild how something so small can connect us all in this epic yearly battle against an invisible foe?