Imagine a world where a simple shot can prevent cancer. Not just reduce your risk, but slam the door shut on the second most common cancer-causing virus in the world. That’s not a sci-fi fantasy—it’s our reality, thanks to the HPV vaccine. It’s a story of scientific breakthrough, passionate advocacy, and fierce debate. It’s also a tale about hope, about saving lives before tragedy can even begin. How did a cancer-preventing vaccine rise from scientific obscurity to become a global milestone? Let’s take a riveting journey through the twists, turns, and triumphs of the HPV vaccine—a shot that has quietly changed the future for millions.
The Hidden Threat of Human Papillomavirus
Ask most people what HPV is, and you’ll get a blank stare. Yet this sneaky virus is everywhere—so common, nearly everyone who’s ever been sexually active will catch it at some point in their lives. Most never know. In many cases, the immune system sweeps it away without a trace. But sometimes, HPV lingers, quietly tampering with the DNA in cells. Years later, this invisible intruder can spark cervical cancer, throat cancer, and several others. It’s a chilling reminder that some of our biggest threats are the ones we can’t see or feel.
Discovery of HPV’s Link to Cancer
The real bombshell dropped in the late 1970s, when German virologist Harald zur Hausen made the shocking connection between HPV and cervical cancer. Until then, scientists suspected a virus might be involved, but zur Hausen’s work proved it. His findings didn’t just shake up cancer biology—they launched a wave of research across the globe. The Nobel Prize he earned in 2008 was well-deserved, but more importantly, it opened the door to prevention. Suddenly, the idea of a vaccine to stop cancer in its tracks wasn’t just wishful thinking.
The Race to Create a Vaccine
Once the link was established, a new question took center stage: Could scientists outsmart HPV before it caused harm? The challenge was daunting. HPV is a master of disguise, with over 200 versions—some harmless, others deadly. Researchers had to figure out which types were the real culprits behind cancer, and then design a vaccine that trained the immune system to fight them off. It was a marathon, not a sprint, filled with trial, error, and countless setbacks. Still, the promise of stopping cancer before it started kept scientists pushing forward.
Pioneering Laboratory Breakthroughs
Early work focused on finding the best way to mimic the virus without causing infection. Researchers learned to create virus-like particles—essentially harmless shells that looked like HPV to the immune system. This trick fooled the body into mounting a powerful defense, providing immunity without risk. These breakthroughs paved the way for clinical trials, showing that what worked in test tubes could protect people in the real world. It was the scientific equivalent of a magic trick—making something dangerous disappear before it could do any harm.
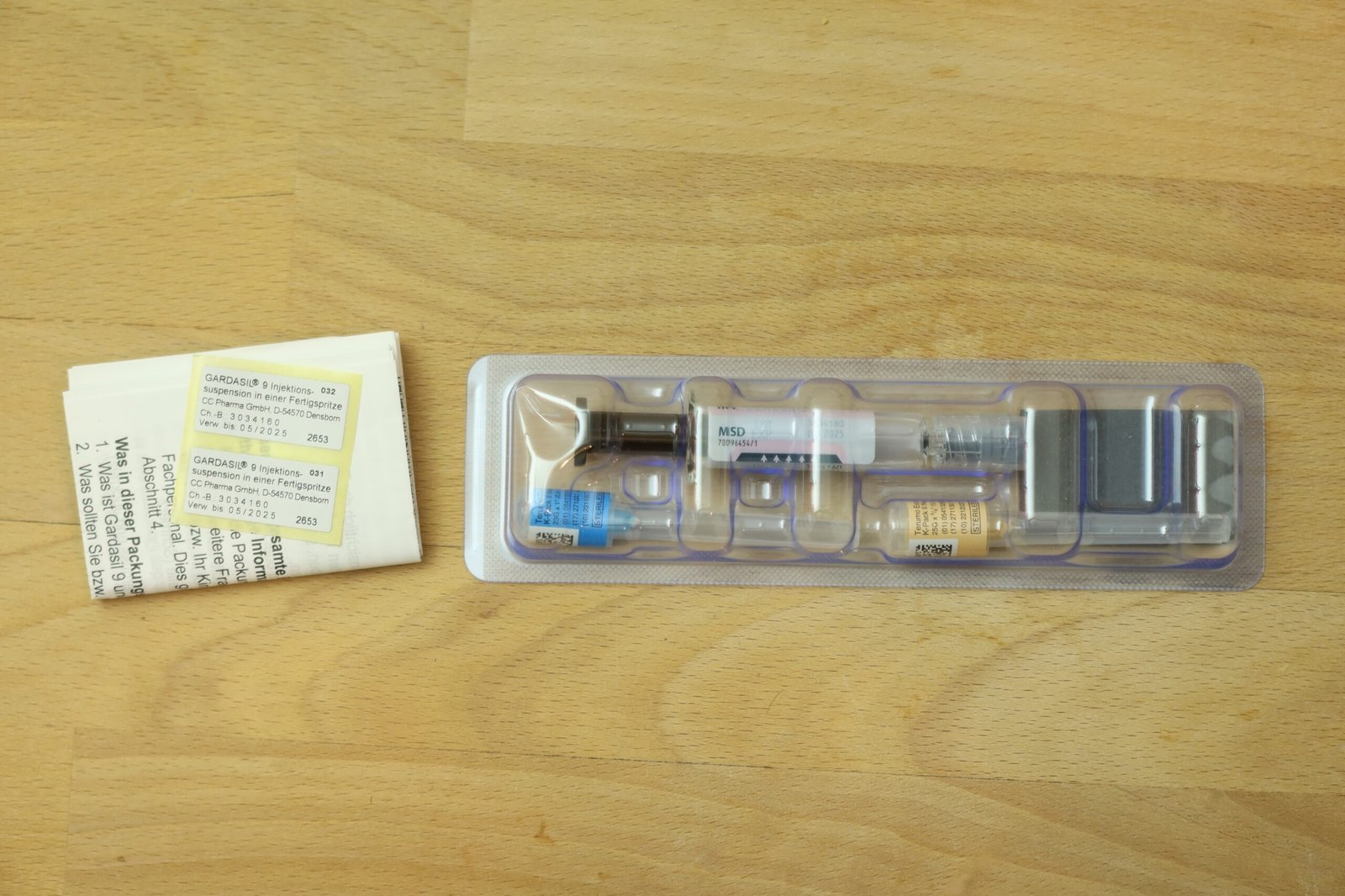
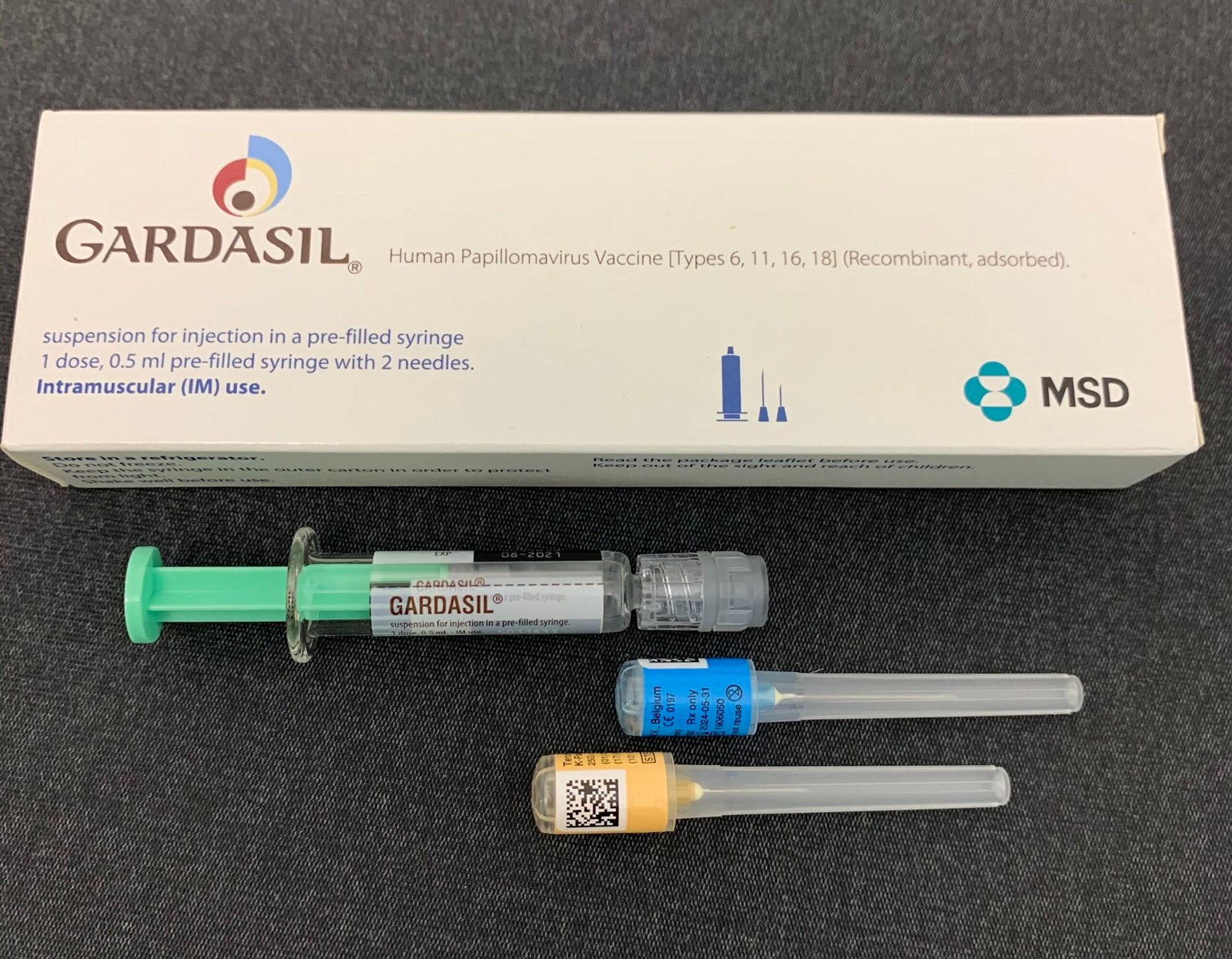
The First HPV Vaccine: Gardasil Hits the Market
In 2006, the world saw a medical milestone: Gardasil, the first HPV vaccine, was approved for use. The excitement was palpable. Gardasil targeted four types of HPV—two that cause most cervical cancers, and two responsible for genital warts. The shot quickly became a symbol of hope, especially for young women. For the first time, a vaccine could stop cancer before it even started. Parents, doctors, and public health leaders celebrated, knowing this was the dawn of a new era in cancer prevention.
Cervarix and Expanded Protection
Not long after Gardasil, another vaccine entered the scene: Cervarix. Approved in 2009, Cervarix honed in on the two most dangerous HPV types linked to cervical cancer. While it didn’t protect against genital warts, it offered robust cancer protection and an alternative for those who couldn’t take Gardasil. Having more than one vaccine meant better access and more choices—crucial steps in the battle against HPV-related cancers. The arsenal was growing, and so was hope.
HPV Vaccines for Boys: A Paradigm Shift
At first, HPV vaccines were aimed squarely at girls. But as research piled up, it became clear that boys needed protection too. HPV doesn’t care about gender—it causes throat, anal, and penile cancers as well. In 2011, health authorities in several countries began recommending the vaccine for boys. This wasn’t just about fairness; it was about shutting down the virus’s ability to spread. By vaccinating both sexes, communities could achieve “herd immunity,” slashing infection rates across the board. It was a bold, science-backed move that changed the conversation forever.
Myths, Misconceptions, and Fierce Debates
No scientific breakthrough comes without controversy. From the start, the HPV vaccine faced a barrage of myths: claims that it encouraged risky behavior, that it was unsafe, or that it wasn’t necessary. Some parents hesitated, worried about side effects. Despite overwhelming evidence that the vaccine is safe and effective, misinformation spread like wildfire in some circles. The debates were emotional, sometimes political, and often left families caught in the crossfire. But beneath the noise, the scientific facts stood firm—this was a vaccine that could save lives.
Real-World Impact: Declining Cancer Rates
A decade after the first shots, the results began rolling in—and they were nothing short of inspiring. Countries with high vaccination rates saw dramatic drops in HPV infections, precancerous lesions, and cervical cancer cases. In Australia, for example, experts now predict cervical cancer could be virtually eliminated within a generation. The numbers tell a powerful story: vaccines work. They’re not just a theory—they’re changing lives, and in some cases, rewriting the future of public health.
Vaccine Access: Global Challenges and Triumphs
While high-income countries have made great strides, millions in low- and middle-income nations still lack easy access to the HPV vaccine. The reasons are complex: high costs, supply shortages, and logistical barriers. Yet, global organizations are fighting to close the gap. Partnerships and innovative programs are bringing vaccines to schools, clinics, and remote villages. Every dose given is a victory against cancer, and the momentum keeps building. The vision is simple: a world where birthplace doesn’t determine cancer risk.
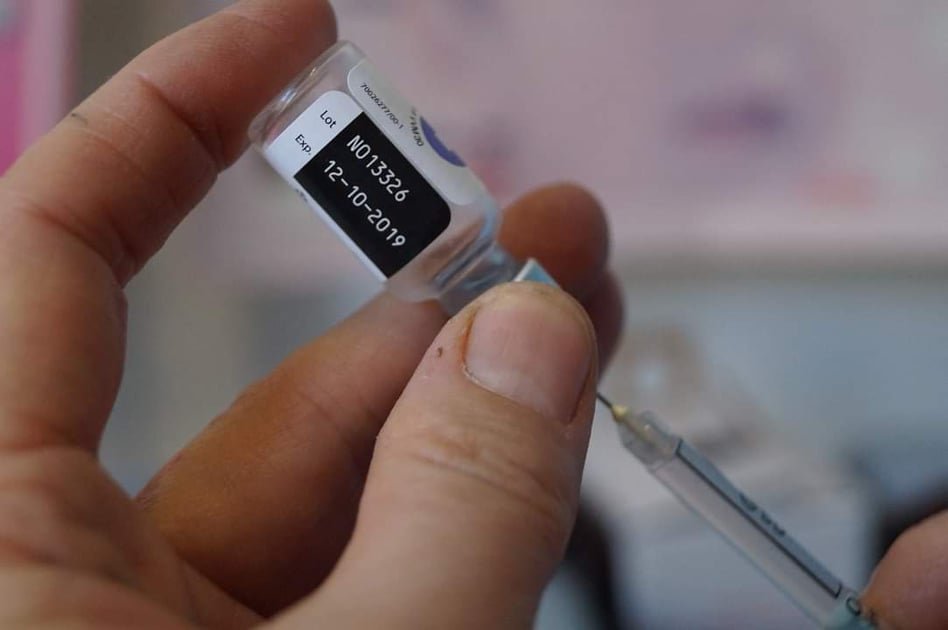
Dosing Schedules: Simplifying Protection

Originally, the HPV vaccine required three shots over six months. For busy families, this was a hurdle. But new research showed that two doses, or even a single dose in some cases, could offer strong protection. This discovery was a game-changer, making it easier for kids and teens—and their parents—to complete the series. The change also stretched vaccine supplies further, allowing more young people to get protected with fewer resources. Sometimes, less really is more.
Expanding Age Recommendations
When the HPV vaccine debuted, it was reserved for preteens and teens. But studies revealed that older teens and young adults could still benefit. Today, people up to age 26—and in some cases, even those in their mid-40s—are eligible. While earlier is still better, the opportunity for “catch-up” vaccination gives more people a second chance. This flexibility has meant more lives protected, and more opportunities to stop cancer before it starts.
HPV Vaccines and Other Cancers
Most people associate HPV with cervical cancer, but the virus is also a leading cause of cancers of the anus, penis, vulva, vagina, and the back of the throat. Recent studies have spotlighted these other risks, pushing the conversation beyond women’s health. The HPV vaccine’s ability to prevent these cancers in both men and women underscores its importance. It’s not just about one disease or one group—it’s about stopping a whole family of cancers in their tracks.
Voices of Survivors and Advocates
Perhaps the most powerful part of the HPV vaccine’s story comes from survivors and advocates. People who lost loved ones to preventable cancers, or who survived cancer themselves, have become some of the vaccine’s fiercest champions. Their stories are raw and real—a reminder that behind every statistic is a person, a family, a life changed forever. Listening to these voices drives home what’s at stake and why the fight for vaccination matters so much.
HPV Vaccination and Social Equity
The HPV vaccine shines a light on bigger questions of fairness and access. In many places, vulnerable groups—like those with lower incomes or less education—are less likely to be vaccinated. This deepens health inequalities that already exist. Efforts to make the vaccine available in schools, public clinics, and rural areas are helping to level the playing field. The fight against HPV is also a fight for a more just, healthier world.
The Role of Schools and Public Health Campaigns
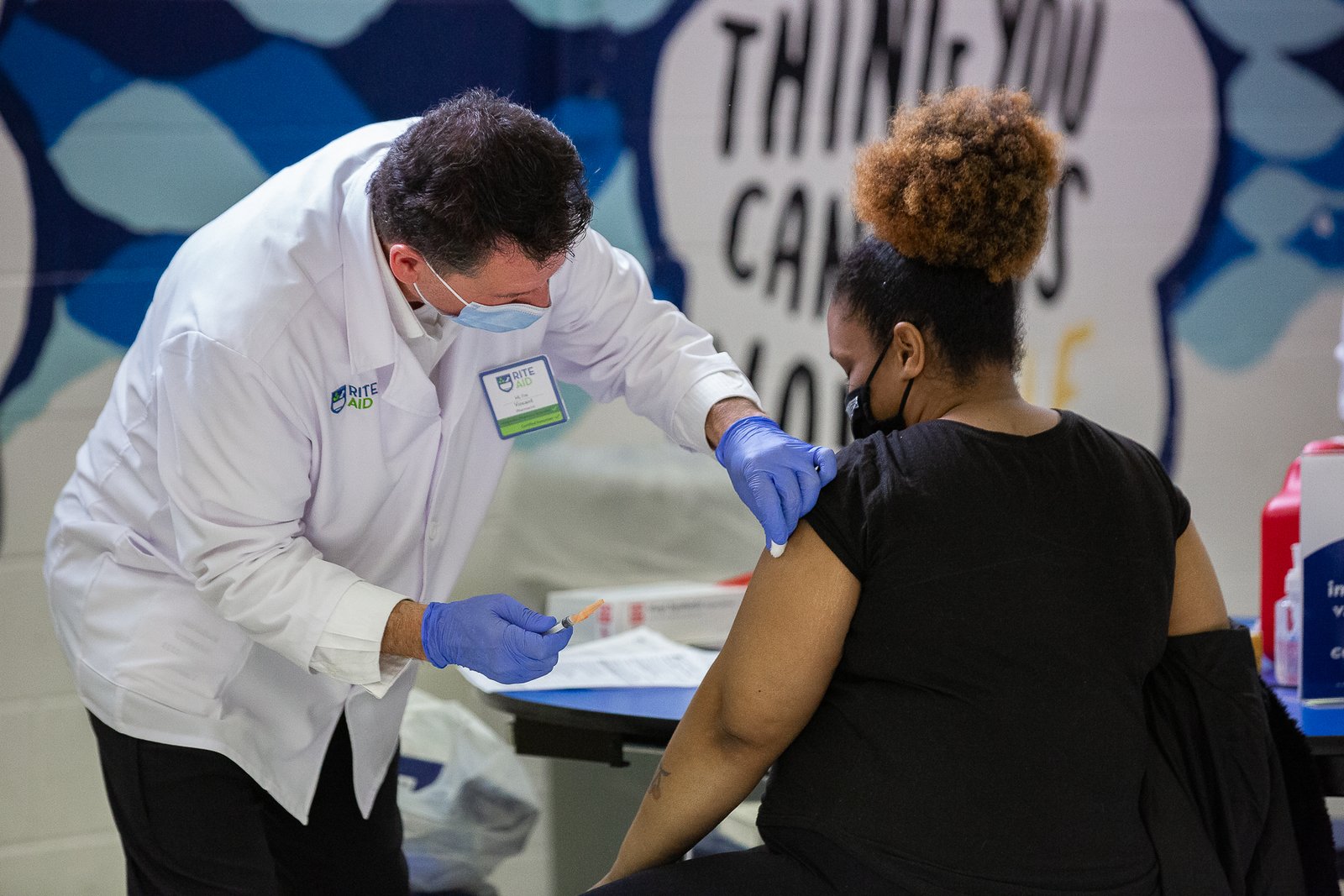
Getting vaccines into arms isn’t just a medical challenge—it’s a social one. Schools have become critical battlegrounds. Many countries offer HPV vaccines as part of school health programs, making it easy and convenient for kids to get protected. Public health campaigns, featuring everything from celebrity endorsements to eye-catching posters, aim to educate and persuade. The message is clear: this vaccine is safe, effective, and can save lives.
Breakthrough Research: Next-Generation Vaccines

Science never stands still. Researchers are already working on next-generation HPV vaccines that could cover even more virus types and provide longer-lasting immunity. Some are exploring nasal sprays or skin patches instead of shots—making protection even simpler and less scary. Others hope to combine HPV vaccines with other childhood vaccines, streamlining the whole process. It’s an exciting time, with the promise of even better tools just over the horizon.
Stories from the Front Lines: Doctors and Nurses
Healthcare workers see firsthand the heartbreak that cancer brings—and the hope that vaccines offer. Many doctors and nurses have powerful stories of kids getting their shots, parents asking tough questions, and communities rallying together. Their dedication is infectious. They’re not just giving medicine; they’re building trust, answering fears, and sometimes even wiping away tears. Without these everyday heroes, the story of the HPV vaccine wouldn’t be possible.
HPV Vaccines in a Post-Pandemic World
The COVID-19 pandemic disrupted vaccination programs everywhere, including HPV. Many kids missed routine shots, and some programs were paused. Now, there’s a renewed urgency to catch up and keep moving forward. Health officials are doubling down, determined that a temporary setback won’t undo years of progress. The HPV vaccine’s journey is a testament to resilience and adaptability, even in the face of global upheaval.
The Road Ahead: Toward a Cancer-Free Generation

The story of the HPV vaccine isn’t finished. Today, millions of young people are protected, but millions more still need access. The science is clear, the impact is undeniable, and the mission is urgent. Each shot given is a step closer to a world where cancer caused by HPV is a distant memory. Will the next generation look back in disbelief that these cancers ever existed? The answer lies in the choices we make today.




