Antibiotic resistance is a growing threat worldwide, posing serious risks to public health, agriculture, and the economy. As bacteria evolve into superbugs resistant to multiple antibiotics, we are increasingly at risk of entering a post-antibiotic era where common infections could become lethal once again. Understanding how superbugs develop and discovering effective strategies to combat antibiotic resistance are crucial steps in safeguarding future generations.
Evolution of Superbugs

The evolution of superbugs is a natural consequence of antibiotic use. Each time antibiotics are used, sensitive bacteria are killed, but a few resistant ones may survive and multiply. Over time, these resistant bacteria can thrive and spread, especially in environments where antibiotic exposure is frequent. This evolutionary process is accelerated by the overuse and misuse of antibiotics in humans and animals, contributing to the rise of these formidable pathogens known as superbugs.
Common Types of Superbugs
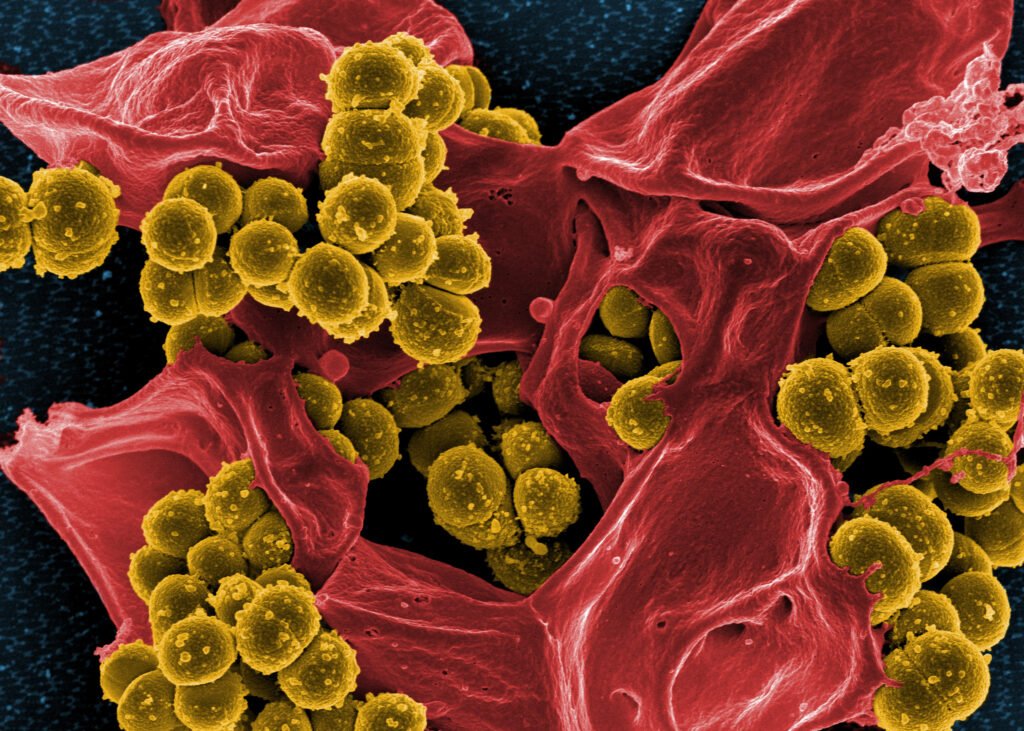
Some of the most concerning superbugs include Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococci (VRE), and carbapenem-resistant Enterobacteriaceae. These bacteria have evolved mechanisms to resist multiple, often last-resort, antibiotics, making infections difficult to treat. MRSA, for instance, has become common in hospital settings but is also appearing in the community at large.
The Role of Antibiotic Overuse

One of the main drivers of antibiotic resistance is the overuse and misuse of these drugs. In many countries, antibiotics are prescribed excessively or used inappropriately, such as for viral infections against which they are ineffective. Additionally, the use of antibiotics in agriculture to promote growth in livestock contributes significantly to the problem, allowing resistant bacteria to enter the food chain and environment.
Impact on Global Health

The rise of antibiotic-resistant bacteria poses a severe threat to global health. Without effective antibiotics, the mortality rate from infectious diseases like tuberculosis, pneumonia, and sepsis is expected to increase dramatically. Furthermore, medical procedures such as surgeries and chemotherapy, which rely on antibiotics to prevent infection, will become much riskier.
Current Efforts to Combat Superbugs

Scientists and healthcare professionals around the world are taking action to combat antibiotic resistance. This includes developing new antibiotics, improving diagnostic tools to ensure appropriate use of existing treatments, and promoting global awareness about the prudent use of antibiotics. Research is also underway to explore alternative treatment methods, such as bacteriophage therapy and immune-based therapies.
The Importance of Surveillance

Effective monitoring and surveillance systems are critical in managing antibiotic resistance. By tracking the prevalence and spread of superbugs, health authorities can respond more effectively to outbreaks. Surveillance data also help in identifying emerging resistance patterns and in guiding the use of antibiotics.
Education and Public Awareness

Raising public awareness about the risks of antibiotic misuse is key to curbing resistance. Educational campaigns can inform the public about the importance of following prescriptions properly and the dangers of self-medicating. Engaging healthcare professionals in continuous education programs can ensure the rational prescribing of antibiotics.
Reducing Agricultural Antibiotic Use

In agriculture, reducing the use of antibiotics vital to human medicine is essential. Implementing more stringent regulations and providing incentives for the development of antibiotic alternatives in livestock production can help reduce reliance on these drugs. Promoting better animal husbandry and hygiene practices also plays a crucial role in this effort.
Promoting Research and Development

Investing in the research and development of new antibiotics and alternative treatments is fundamental to staying ahead of superbugs. Encouraging public-private partnerships and offering financial incentives for pharmaceutical companies to research new drugs can revitalize the antibiotic pipeline.
Strengthening Infection Control

Hospitals and healthcare facilities can implement stringent infection control measures to prevent the spread of resistant bacteria. This includes enforcing hand hygiene, sterilizing medical equipment, and isolating infected patients. Such measures are vital in curbing the transmission of superbugs in healthcare settings.
Adopting a Global Strategy

Antibiotic resistance is a global issue that requires coordinated international action. The World Health Organization and other international bodies are working to develop a comprehensive strategy that includes surveillance, prevention, research, and regulation to tackle antibiotic resistance globally.
Personal Responsibility in Preventing Superbugs

Individuals can make a difference by using antibiotics responsibly. This involves following healthcare providers’ advice, not demanding antibiotics for viral infections like colds and flu, and avoiding the use of leftover prescriptions. Personal responsibility and informed decision-making can significantly impact the fight against antibiotic resistance.
Conclusion

Antibiotic resistance is a formidable challenge that threatens to undermine decades of medical progress. To combat the evolution of superbugs, a multifaceted approach incorporating prudent antibiotic use, improved infection control, and robust research and development is essential. By implementing effective strategies and fostering global collaboration, we can slow the progression of antibiotic resistance and protect future generations from the devastating impacts of superbugs.