We tend to think of the human body as a finished blueprint, mapped down to the last molecule. But step inside today’s labs and scanning rooms, and that neat picture falls apart in the best possible way. Under our skin, researchers are still stumbling on new structures, previously unseen cell types, and bizarre defense systems that look almost alien. Each discovery rewrites old textbook chapters and raises unsettling questions: how much do we really know about the thing we live inside every day? From secret organs to brainless immune “memories,” the body keeps revealing that it is less a static machine and more a restless, evolving ecosystem we barely understand.
The Glymphatic Night Shift: Your Brain’s Hidden Cleaning Crew

Imagine if your city only took the trash out at night, using a network of hidden back alleys you never see in daylight. That is roughly what neuroscientists have realized the brain is doing through the so‑called glymphatic system, a fluid-clearing network that ramps up while you sleep. Instead of relying only on blood vessels, cerebrospinal fluid flows along channels wrapped around veins and arteries, flushing away metabolic waste, including proteins linked to Alzheimer’s disease. The catch is that this system works dramatically better when you are in deep, high‑quality sleep, particularly slow‑wave sleep. That makes bedtime feel less like a luxury and more like a critical maintenance window your brain cannot afford to skip.
Researchers are now racing to understand how lifestyle, age, and disease alter this hidden plumbing. Early studies suggest that disrupted sleep may slow the nighttime flow, letting toxic by‑products accumulate over years. There are also hints that head position during sleep might slightly change how efficiently fluid drains, leading to some provocative but still debated experiments about side sleeping and brain health. For now, the bigger message is plain: treating sleep like an optional extra could be quietly sabotaging one of the brain’s most important self‑cleaning tools.
New Cells, New Rules: The Immune System’s Shape‑Shifting Players

If you learned basic immunology in school, you probably heard a simple cast list: T cells, B cells, maybe a few natural killer cells patrolling like tiny security guards. Over the past decade, that neat roll call has exploded as scientists have uncovered whole new families of immune cells with strange hybrid roles. A standout example is the group known as innate lymphoid cells, which blur the line between the fast, blunt innate immune response and the more targeted adaptive one. These cells cluster in tissues like the gut and lungs, reacting within hours to threats, yet shaping long‑term immune balance as well.
On top of that, researchers have mapped specialized T cell subtypes tucked into nearly every organ, each tuned to that tissue’s unique dangers and needs. Some can switch from defenders to potential troublemakers, driving chronic inflammation if they are not properly restrained. A few years ago, I sat in on a conference session where several teams admitted, half‑jokingly, that the immune system’s cell map now looks more like a galaxy catalog than a neat family tree. This matters in real life: the more we learn about these hidden players, the more targeted therapies we can design for autoimmune diseases, allergies, and even cancer, moving beyond blanket immune suppression to surgical‑precision tuning.
The Microbiome’s Dark Corners: Viruses, Fungi, and the Ghostly “Virome”

Most of us have heard the basic microbiome story by now: trillions of bacteria in the gut help digest food and train the immune system. Yet that is only the brightest layer of a much stranger ecosystem. Nestled among those bacteria are vast communities of viruses that infect microbes rather than human cells, along with fungi and other tiny organisms that are harder to grow and study. Collectively, this under-sampled layer is sometimes called the virome and mycobiome, and it is turning out to be just as important as the bacteria we first focused on. Early findings point to viral “shepherds” that keep bacterial populations in check, and fungal blooms that may accompany or drive inflammation in conditions like inflammatory bowel disease.
What is startling is how dynamic this hidden world is. A course of antibiotics, a major diet change, or even travel to a new region can shift these viral and fungal populations, sometimes in ways that persist for months or years. Preliminary research suggests that specific viral communities might predict who responds well to certain cancer immunotherapies. At the same time, there is growing concern about over‑promising probiotic fixes when we still cannot fully see or control the deeper layers of this ecosystem. The real frontier is not a single “good” gut bug in a capsule, but learning how to nudge these complex, layered communities back into balance without unexpected side effects.
The Body’s Electrical Whisper Network: Hidden Bioelectric Codes

When we talk about electricity in the body, we usually mean neurons firing in the brain or signals racing down nerves to move a muscle. But biologists are uncovering a quieter, more widespread electrical language written into the membranes of nearly every cell. Tiny voltage differences across cell membranes seem to guide how tissues grow, repair, and even decide what shape to take. In regeneration research, for instance, changing the bioelectric pattern in a wound can sometimes coax cells to rebuild structures more faithfully, like a subtle blueprint coded in voltage rather than DNA.
This bioelectric whisper network has sparked bold ideas: if we can read and modulate these patterns, could we encourage better healing after injury, or even limit cancer growth by resetting aberrant signals? Experimental work in animals has already shown that tweaking voltage gradients can alter limb development and organ formation. Translating that to humans will be far more complex and ethically fraught, but the concept alone is transformative. It suggests that genes are only one part of the story, and that the body carries an additional, electrical layer of instruction that we are just beginning to decode.
The Hidden Clues in Connective Tissue: Fascia as a Sensing Superweb

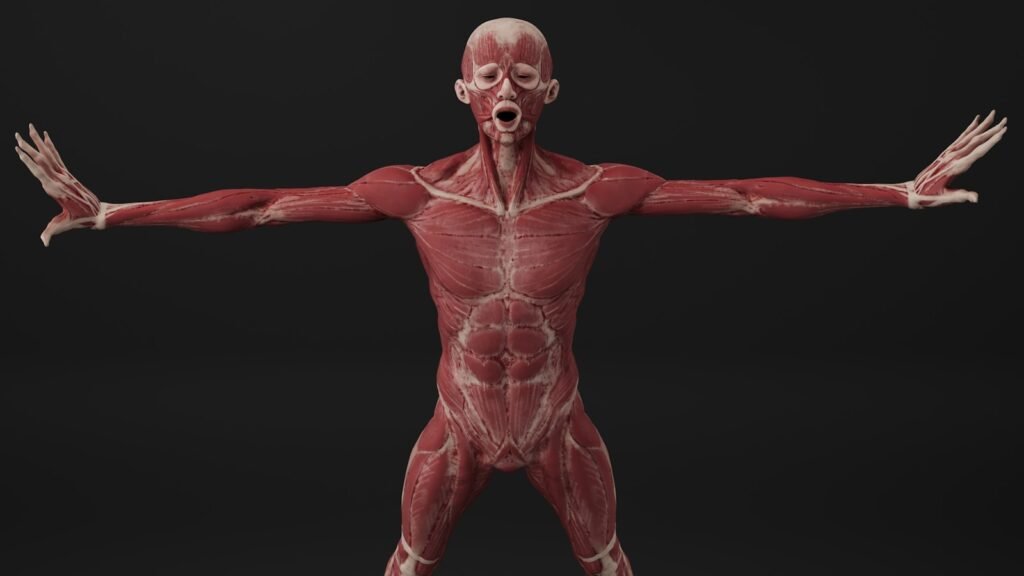
For decades, fascia – the thin sheets and bands of connective tissue wrapping muscles and organs – was treated as anatomical packing material, something surgeons cut through to get to the “important” parts. Recent research has flipped that dismissive view on its head. Fascia is laced with nerve endings, immune cells, and blood vessels, forming a continuous tension‑bearing web from head to toe. Instead of being passive wrapping, it acts more like a dynamic sensory organ, helping the body track movement, posture, and even subtle internal stresses.
Some pain researchers now suspect that chronic, poorly localized pain may arise when fascia stiffens, scars, or becomes inflamed, disrupting how forces and signals travel through this web. Studies using ultrasound and MRI are revealing how fascia glides – or fails to glide – over muscles during motion, hinting at new diagnostics for overuse injuries and long‑standing back pain. This has practical implications for everything from physical therapy to surgical techniques, where preserving or restoring healthy fascial planes might speed recovery. In a way, we are only now learning to “see” a structure that was in every anatomy diagram all along, hiding in plain sight as a silent coordinator of movement and sensation.
From Ancient Tools to Modern Science: The Lymphatic System’s Secret Pathways

Healers have been pressing, massaging, and draining swollen limbs for thousands of years, intuitively working with the lymphatic system long before anyone could see it. Yet even in the twenty‑first century, key parts of this fluid‑clearing network went unnoticed until advanced imaging caught them. One of the most startling updates came when scientists confirmed functional lymphatic vessels in the membranes surrounding the brain, overturning a long‑held belief that the brain lacked classic lymph drains. That finding instantly reframed how researchers think about brain inflammation, waste clearance, and diseases like multiple sclerosis.
Modern tools now let researchers trace lymph flow in real time, revealing complex regional circuits that interact with immune responses and even fat metabolism. Techniques that once seemed purely “alternative,” like gentle lymph‑focused massage, are being revisited with more rigorous clinical trials to see which approaches actually improve fluid movement and reduce swelling. At the same time, new drugs and devices aim to prevent or treat lymphedema, a painful swelling that can follow cancer surgery or radiation when lymph channels are damaged. It is a striking example of old hands‑on knowledge finally meeting detailed biological maps, with both sides pushing our understanding forward.
Why It Matters: Rethinking the “Known” Human Body

All of these discoveries strike at the comforting belief that we had basically finished mapping the human body sometime in the last century. Instead, they show that our internal world is more like an unexplored ocean, where each new trench or reef changes how we navigate the whole. When researchers uncover a new cleaning system in the brain, a hidden sensory web in fascia, or unexplored immune players, it does not just add trivia to a textbook. It reshapes how we diagnose disease, when we intervene, and which symptoms we even take seriously in the first place. People living with conditions once dismissed as “all in your head” may suddenly find their experiences grounded in newly visible biology.
Compared with traditional views that treated organs as isolated machines, this emerging picture emphasizes networks, feedback loops, and ecosystems. It highlights how sleep, movement, diet, stress, and environment tug on hidden levers we did not know existed. That has big implications for medicine: instead of waiting for organs to fail and then replacing parts, there is a growing push to maintain these quiet systems long before breakdown. For patients, it means that listening carefully to subtle bodily changes is not overreacting – it might be the only way to catch early signals from systems we are just now equipped to understand.
The Future Landscape: Mapping the Last Frontiers Under Our Skin

Looking ahead, the most transformative tools may be those that let us see the living body in motion, down to the single cell. High‑resolution imaging, advanced MRI techniques, and molecular tagging already allow scientists to watch immune cells swarm, lymphatic fluid pulse, or fascia stretch in a breathing, moving human. Paired with powerful computational models, this could create dynamic “digital twins” of our bodies that predict how hidden systems will respond to a drug, surgery, or lifestyle shift. It is an enticing vision, but it comes bundled with serious questions about privacy, access, and who gets to benefit from such fine‑grained biological insight.
On the lab bench, organ‑on‑a‑chip devices, 3D cell cultures, and microscopic sensors are letting scientists probe bioelectric codes, glymphatic flow, and microbiome shifts in unprecedented detail. Still, there is a real risk of getting dazzled by beautiful data while everyday clinical care lags behind. Global inequities mean that many patients still struggle to access basic diagnostics, let alone cutting‑edge imaging of their lymph vessels or fascia. The challenge for the coming decades will be to translate these hidden wonders into practical, affordable tools that change outcomes, not just headlines. If we can manage that, understanding the body’s secret systems might finally help more of us live not just longer, but better.
Everyday Engagement: How Readers Can Tune In to Their Own Hidden Systems

You do not need a lab coat or a research grant to start engaging with these discoveries in your own life. Paying honest attention to sleep, for example – its timing, depth, and how you feel the next day – is a direct way to support that nighttime glymphatic housekeeping in the brain. Gentle movement practices, from walking to stretching or yoga, help keep fascia, lymph, and circulation responsive rather than sluggish. Feeding the microbiome with a varied, fiber‑rich diet and being mindful of unnecessary antibiotic use respects the complex communities that share your body.
Beyond personal habits, there is power in curiosity and support. Following reputable science coverage, backing medical research charities, or even participating in ethical clinical studies when appropriate can push this field forward. When you do see a doctor, asking questions about sleep, pain patterns, or gut changes can gently nudge conversations toward these emerging systems rather than just isolated lab numbers. In the end, staying curious about your own biology is not self‑indulgent – it is a way of voting for a future where medicine treats the body not as a black box, but as a living landscape we are still learning to read.

Suhail Ahmed is a passionate digital professional and nature enthusiast with over 8 years of experience in content strategy, SEO, web development, and digital operations. Alongside his freelance journey, Suhail actively contributes to nature and wildlife platforms like Discover Wildlife, where he channels his curiosity for the planet into engaging, educational storytelling.
With a strong background in managing digital ecosystems — from ecommerce stores and WordPress websites to social media and automation — Suhail merges technical precision with creative insight. His content reflects a rare balance: SEO-friendly yet deeply human, data-informed yet emotionally resonant.
Driven by a love for discovery and storytelling, Suhail believes in using digital platforms to amplify causes that matter — especially those protecting Earth’s biodiversity and inspiring sustainable living. Whether he’s managing online projects or crafting wildlife content, his goal remains the same: to inform, inspire, and leave a positive digital footprint.