The salamander doesn’t mourn its lost tail. Within weeks, it simply grows a new one. No surgery, no prosthetics, no adaptation period – just pure biological magic that leaves scientists wondering why humans can’t do the same thing. While we’ve mastered heart transplants and brain surgery, regrowing a lost arm or leg remains one of medicine’s most elusive dreams. But across America, brilliant researchers are pushing the boundaries of what we thought possible, and they’re getting closer to cracking the code of human regeneration.
The Revolutionary Science Behind Limb Regeneration

Human limb regeneration isn’t science fiction anymore – it’s becoming scientific reality. The process involves reprogramming adult cells to behave like embryonic stem cells, creating what scientists call a “regenerative niche.” This microscopic environment signals damaged tissue to rebuild itself from scratch, much like how a lizard regrows its tail. The challenge lies in convincing human cells, which naturally form scar tissue after injury, to instead form new bones, muscles, nerves, and blood vessels. Recent breakthroughs in gene therapy and tissue engineering are making this cellular reprogramming possible for the first time in human history.
Wake Forest Institute for Regenerative Medicine – North Carolina

Dr. Anthony Atala’s team at Wake Forest has already achieved the impossible – they’ve grown human organs in laboratories. Their latest project focuses on bioprinting entire limb structures using a patient’s own cells as building blocks. The lab’s 3D bioprinters can create scaffolds that perfectly match a patient’s anatomy, then seed these frameworks with stem cells that grow into functional tissue. What makes their approach unique is their ability to print multiple tissue types simultaneously, creating complex structures with blood vessels, nerves, and muscle fibers all in one process. Their recent success with printing skin grafts for burn victims has paved the way for more ambitious limb regeneration projects.
Harvard’s Wyss Institute – Massachusetts

The Wyss Institute takes inspiration directly from nature’s best regenerators. Scientists here study axolotls, those adorable Mexican salamanders that can regrow entire limbs in just a few months. By identifying the specific genes that trigger regeneration in these creatures, researchers are developing ways to activate similar pathways in human cells. Their breakthrough discovery involves a protein called MSX1, which acts like a master switch for regeneration. When they introduced this protein into mouse cells, the animals showed unprecedented healing abilities, regrowing fingertips complete with bone, muscle, and even fingerprints.
Johns Hopkins Applied Physics Laboratory – Maryland

While others focus on biological solutions, Johns Hopkins is pioneering the integration of artificial and biological systems. Their revolutionary approach combines advanced prosthetics with regenerative medicine to create hybrid limbs that function better than the original. The lab’s neural interface technology allows patients to control artificial limbs with their thoughts, while simultaneously encouraging natural tissue regeneration around the prosthetic. This dual approach means patients get immediate functionality while their body slowly regrows natural tissue. Their recent trials with amputee veterans have shown remarkable success rates, with some patients reporting sensation in their artificial limbs.
University of California San Francisco Gladstone Institutes

UCSF’s approach reads like something from a superhero movie – they’re trying to give humans wolverine-like healing powers. Their research focuses on epigenetic reprogramming, essentially rewriting the cellular instruction manual that tells cells how to behave after injury. By temporarily reverting adult cells to an embryonic-like state, they can trick the body into thinking it’s still developing, triggering massive regenerative responses. Their recent experiments with mice resulted in complete limb regeneration within 60 days, including fully functional bones, muscles, and nervous systems. The team believes human trials could begin within the next five years.
Stanford University School of Medicine – California

Stanford’s regenerative medicine lab has discovered something remarkable about human children – they actually can regenerate fingertips, but only up until about age seven. This finding led researchers to investigate what changes in our bodies that shut down this natural ability. Their current research involves using growth factors and stem cell therapy to reactivate dormant regenerative pathways in adult tissue. The lab recently achieved partial limb regeneration in laboratory models by combining bone marrow stem cells with specific growth hormones. Their work suggests that humans haven’t lost the ability to regenerate – we’ve just forgotten how to turn it on.
MIT Koch Institute for Integrative Cancer Research – Massachusetts

MIT’s approach to limb regeneration came from an unexpected source – cancer research. Scientists noticed that cancer cells possess an almost supernatural ability to grow and spread, hijacking the body’s natural repair mechanisms. By studying these cellular invasion techniques, researchers developed ways to redirect this aggressive growth toward healing instead of harm. Their innovative biomaterial scaffolds can be implanted at amputation sites, where they release controlled doses of growth factors over several months. Early trials show that these scaffolds can encourage the regrowth of bone and soft tissue, with some patients experiencing up to three inches of new limb growth.
The Cellular Reprogramming Revolution

The key to human regeneration lies in understanding how cells make decisions about their future. Every cell in your body contains the same DNA, yet somehow a heart cell knows to beat while a brain cell thinks and a bone cell stays rigid. Scientists are learning to reprogram these cellular destinies using techniques that would have seemed magical just decades ago. The process involves introducing specific transcription factors – molecular switches that can change what genes are turned on or off in any given cell. This reprogramming can transform ordinary skin cells into powerful stem cells capable of becoming any tissue type the body needs.
Bioengineering the Perfect Scaffold

Growing a new limb requires more than just cells – it needs a framework to grow on. Modern bioengineers are creating scaffolds that dissolve away as new tissue forms, leaving behind perfectly structured organs and limbs. These scaffolds aren’t just passive frameworks; they’re programmed to release growth factors, nutrients, and signaling molecules at precisely the right times during development. The most advanced scaffolds can even conduct electrical signals, helping to establish the neural networks that allow movement and sensation. Think of them as temporary construction sites that build themselves into permanent structures.
The Neural Network Challenge

Regrowing muscles and bones is one thing, but reconnecting the incredibly complex network of nerves that control movement and sensation presents an entirely different challenge. The human hand alone contains over 17,000 nerve endings, each precisely connected to create our incredible dexterity and sense of touch. Researchers are developing guidance systems that help regenerating nerves find their correct targets, much like GPS navigation for growing neural pathways. Recent breakthroughs in nerve growth factors and electrical stimulation are showing promise in restoring both motor control and sensory feedback in regenerated tissue.
Stem Cell Therapy Breakthroughs

The discovery of induced pluripotent stem cells revolutionized regenerative medicine by allowing scientists to create powerful stem cells from ordinary adult tissue. These reprogrammed cells can theoretically become any type of tissue in the human body, making them perfect candidates for limb regeneration. Current research focuses on directing these stem cells to form specific tissue types in the correct proportions and arrangements needed for functional limbs. The challenge lies in preventing these powerful cells from forming tumors while encouraging them to create complex, organized structures like hands and feet.
Gene Therapy and Regenerative Switches

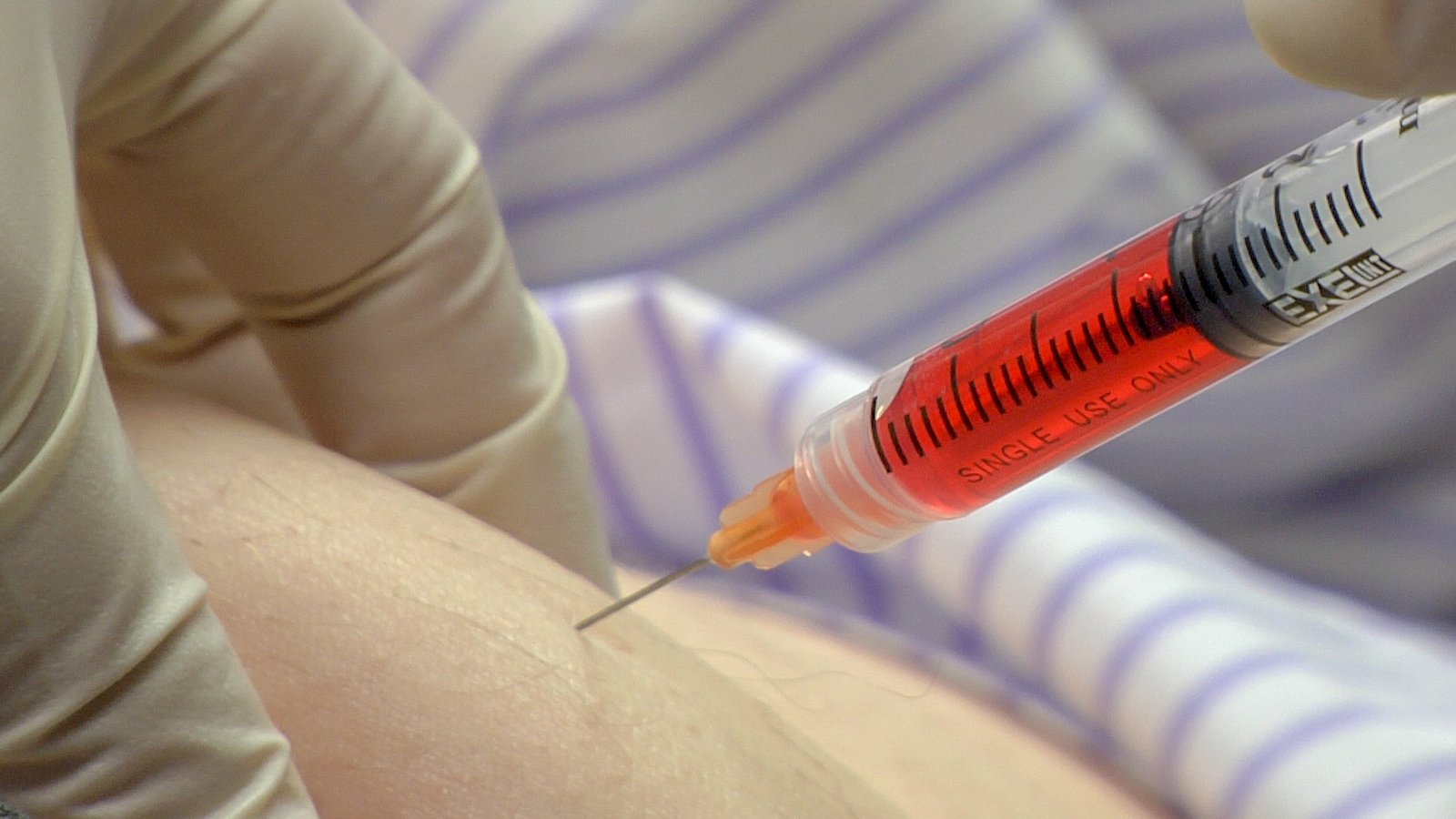
Scientists have identified specific genes that act like master switches for regeneration, and they’re learning how to flip these switches on command. The MSX1 gene, for example, can transform ordinary healing into extraordinary regeneration when activated properly. Gene therapy vectors can deliver these regenerative instructions directly to injury sites, essentially reprogramming the local cellular environment for massive healing responses. This approach offers the possibility of triggering regeneration without surgery or external devices – just a simple injection that unleashes the body’s hidden regenerative potential.
The Immune System’s Role in Regeneration

Your immune system might be the biggest obstacle to regenerating lost limbs. While it excels at protecting you from infection, it also tends to create scar tissue that blocks regenerative processes. Researchers are discovering ways to temporarily modify immune responses at injury sites, allowing regeneration to proceed without interference. This involves using specialized molecules that calm inflammatory responses while promoting tissue growth. Some of the most promising treatments combine immune modulators with growth factors, creating a healing environment that favors regeneration over scarring.
3D Bioprinting Complex Structures

Modern 3D bioprinters can create living tissue with the same precision that regular printers create documents. These remarkable machines layer living cells, growth factors, and biodegradable materials to build complex three-dimensional structures that grow into functional organs. The latest bioprinters can work with multiple cell types simultaneously, creating tissues with proper blood vessel networks and neural connections. Imagine a printer that could create a replacement hand, complete with bones, muscles, skin, and nerve connections, all perfectly matched to your own anatomy.
Clinical Trials and Human Testing
Several regenerative limb treatments are moving from laboratory benches to hospital beds, with human trials beginning across multiple institutions. These early studies focus on safety and basic effectiveness, typically involving patients with partial amputations or severe tissue damage. The results so far have exceeded many researchers’ expectations, with some patients showing significant tissue regrowth and functional improvement. While complete limb regeneration remains experimental, these trials are proving that human tissue can be convinced to regenerate far more than previously thought possible.
Overcoming the Scar Tissue Barrier

Scar tissue formation is evolution’s quick fix for injuries, but it prevents the kind of organized regeneration needed to rebuild complex structures like limbs. Scientists are developing treatments that can dissolve existing scar tissue while preventing new scars from forming during the regeneration process. These anti-scarring therapies work by blocking specific proteins that signal cells to form fibrous tissue instead of functional organs. Combined with regenerative treatments, anti-scarring approaches are showing remarkable success in allowing damaged tissue to rebuild itself properly.
The Timeline for Human Limb Regeneration

Most experts predict that partial limb regeneration will become available for human patients within the next decade, starting with fingers and progressing to hands and eventually entire arms or legs. The first treatments will likely focus on enhancing natural healing processes rather than complete regeneration from scratch. Full limb regeneration – growing an entire arm or leg from an amputation site – remains further in the future, probably 15-20 years away for routine clinical use. However, the rapid pace of recent breakthroughs suggests these timelines could be significantly shortened if current research trends continue.
Ethical Considerations and Future Implications

The ability to regenerate human limbs raises profound questions about the nature of human enhancement and the limits we should place on medical intervention. If we can regrow lost limbs, should we also be able to improve upon the original design, creating stronger bones or more sensitive nerves? These treatments will likely be expensive initially, raising concerns about medical equity and access to life-changing therapies. The psychological impact of regeneration also deserves consideration – how do people adapt to having body parts that are simultaneously theirs and not theirs, grown in laboratories but integrated into their own biology?
Revolutionary Impact on Veterans and Amputees

Military veterans represent one of the most important potential beneficiary groups for regenerative limb technology, with thousands of service members having lost limbs in recent conflicts. Many of these injuries occurred in young, otherwise healthy individuals who could live for decades with their disabilities. Regenerative treatments could restore not just function but also sensation and natural appearance, potentially eliminating the psychological trauma associated with amputation. The Department of Veterans Affairs has become a major funding source for limb regeneration research, recognizing the transformative potential of these treatments for wounded warriors.
The journey from science fiction to medical reality is accelerating faster than anyone imagined just a few years ago. These six laboratories represent humanity’s best hope for conquering one of medicine’s final frontiers, and their combined efforts are bringing us closer to a world where losing a limb doesn’t mean living with permanent disability. The salamander’s secret is finally being unlocked, and soon it might become our own superpower. What would you do with the ability to regrow what you’ve lost?




