Imagine waking up to a notification that quietly whispers your likely cause of death, or a digital assistant reminding you to avoid risky behaviors based on its calculations of your mortality. It sounds like the plot of a futuristic thriller, but this chilling prospect might soon be reality. Algorithms are already learning to predict not only our diseases, but even the likely timing and manner of our deaths. This isn’t science fiction—this is the rapidly approaching frontier of predictive healthcare. As unsettling as it may feel, the idea of machines foreseeing our final moments is capturing the imagination of doctors, scientists, ethicists, and ordinary people. Are we on the brink of conquering fate, or are we opening the door to a new kind of digital determinism? Let’s unravel the electrifying, eerie, and deeply human tale of algorithms that dare to predict the end.
The Rise of Predictive Healthcare
Predictive healthcare is no longer a distant dream but a growing reality in hospitals and clinics worldwide. With vast amounts of medical data now digitized, artificial intelligence (AI) systems can analyze patterns that have long eluded human eyes. These tools are already helping doctors spot diseases like cancer earlier, suggest personalized treatments, and even anticipate complications before symptoms appear. The ability to predict health outcomes is transforming how we approach medicine, shifting the focus from reaction to prevention. It’s as if medicine is evolving from a fire brigade to a team of watchful sentinels. This shift, while promising, brings with it profound questions about privacy, ethics, and the very nature of fate.
How Algorithms Learn to Predict Death
It might sound macabre, but teaching algorithms to predict death starts with feeding them massive datasets: hospital records, diagnostic images, genetic sequences, and lifestyle logs. Machine learning models sift through millions of variables—age, blood pressure, cholesterol, family history, and even subtle clues hidden in lab results. By analyzing which combinations of factors led to mortality in the past, these programs learn to spot the warning signs in new patients. The more data they consume, the sharper their predictions become. It’s a relentless numbers game, with life and death as the stakes.
From Risk Scores to Death Timelines
Doctors have long used risk scores—numbers that estimate your odds of heart attack, stroke, or cancer. What’s new is the precision and reach of today’s AI-powered predictions. Some algorithms now go beyond risk scores, generating personalized death timelines: estimates of not just if, but when and how you might die. For instance, researchers have developed models that predict heart failure patients’ survival to within months, based on subtle changes in test results. This level of granularity is both fascinating and unnerving, raising questions about how much we really want to know about our own mortality.
The Power—and Peril—of Early Warnings
On one hand, knowing your mortality risk could empower you to change your habits, seek treatment sooner, or even make peace with life’s fragility. Imagine a smoker quitting because an algorithm predicts their death within five years, or a patient taking their heart medication more seriously after seeing their odds laid bare. Yet these predictions can also cast a long shadow. Some people may feel doomed by a statistical forecast, slipping into anxiety or fatalism. The power of early warning is double-edged, offering both hope and fear.
Real-World Examples: AI in Action
Hospitals around the world are already putting death-predicting algorithms to work. In the United States, some health systems use AI to flag patients at high risk of dying within the next year, prompting doctors to discuss palliative care options. In the UK, researchers have built models that predict mortality in COVID-19 patients, helping prioritize scarce resources. These successes are inspiring, but they also reveal the delicate balance between saving lives and respecting human dignity. Sometimes, the cold logic of algorithms clashes with the messy emotions of real life.
Can We Trust the Machine?
Trust in algorithms is a fragile thing. When an AI predicts your death, you want to know it’s not guessing or making mistakes. Yet even the best models can be fooled by missing data, biased samples, or unexpected changes in your health. A prediction is only as good as the data it’s trained on—and medical records are often incomplete or skewed. The risk of false alarms, missed diagnoses, or overconfident prognoses is real. For every life saved by an early warning, another patient might suffer needless worry or medical interventions.
The Ethics of Knowing Your Fate
Should you have the right to know your predicted death date? Or should such knowledge be kept from you, to protect your mental health? The ethics of predictive healthcare are deeply murky. Some argue that patients should be fully informed, empowered to make choices about their future. Others worry that such information could lead to discrimination, despair, or even insurance denial. The prospect of predicting death raises old philosophical questions in new digital forms: How much should we know about the future? And who decides?
Privacy in the Age of Predictive Death

With algorithms crunching through reams of personal data, privacy becomes more precious—and more precarious—than ever before. Medical records, genetic information, and even wearable device data can all feed into death predictions. Who owns this data? How is it protected? The risk of leaks or misuse is real, as is the temptation for companies to profit from your most intimate secrets. The specter of surveillance medicine looms large, where every heartbeat, step, and slip is tracked and tallied.
The Human Reaction: Anxiety, Relief, or Denial?
How do people react when told they have a high chance of dying soon? Responses range from panic and denial to relief and resolve. Some patients become anxious, haunted by their digital death sentence. Others shrug it off, determined to live life on their own terms. A few find comfort in the clarity, using the knowledge to plan for their families or pursue long-postponed dreams. The human heart remains unpredictable, even in the age of algorithms.
Doctors and Death Predictions: Help or Hindrance?
For doctors, predictive algorithms are both a blessing and a burden. These tools can help identify at-risk patients, prompt crucial conversations, and support difficult decisions. But they can also cause confusion, second-guessing, and even conflict with families. Some physicians worry about over-reliance on black-box models that they don’t fully understand. The relationship between doctor, patient, and machine is being rewritten in real time, with trust—and life itself—hanging in the balance.
Predicting Death in the Elderly
Elderly patients often face complex health challenges, making predictions especially valuable—and sensitive. Algorithms can help prioritize care, avoid unnecessary hospitalizations, and support end-of-life planning. Yet these predictions can also feel like a verdict, overshadowing the joys and surprises that can still come in old age. For some seniors, knowing their likely fate brings closure; for others, it brings only fear. The challenge is to use these tools wisely, honoring both the science and the soul.
Insurance, Employment, and the Risk of Discrimination
If algorithms can predict who is likely to die soon, will insurers or employers use this information against us? The answer is already taking shape. Some insurance companies are exploring AI to price policies more accurately—or to deny coverage altogether. Employers may be tempted to screen candidates based on health risks. The potential for discrimination is staggering, threatening to turn our most private fears into barriers to opportunity. Laws and safeguards are still catching up with the pace of technology.
The “Black Box” Problem
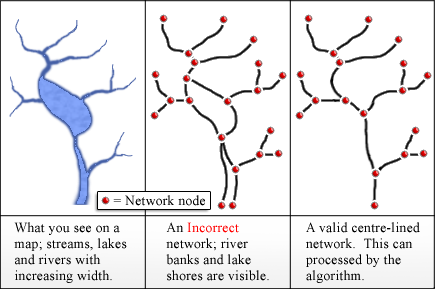
Many death-predicting algorithms are so complex that even their creators can’t fully explain how they work. This “black box” problem makes it hard to challenge or understand a prediction. If a computer says you have six months to live, but can’t say why, should you trust it? The lack of transparency can erode confidence and make it harder for patients and doctors to make informed decisions. Demanding more explainable AI is crucial if we want to use these tools wisely.
Culture, Religion, and Acceptance of Digital Fate
Different cultures and religions view death differently, and the idea of predicting one’s time to die can spark everything from fascination to outrage. In some traditions, only the divine can know the day of our passing; in others, seeking this knowledge is taboo. The arrival of algorithmic death predictions will challenge cultural norms and force societies to grapple with questions of destiny, free will, and the meaning of a good life. Not everyone will welcome these digital prophecies.
Potential Benefits: A Longer, Healthier Life?
Despite the fears, predictive algorithms hold real promise. By identifying risks early, they can help people change course—quitting smoking, eating better, or getting screened for disease. Doctors can tailor treatments to each patient’s unique profile, potentially adding years to life and life to years. The dream is a future where death predictions don’t just forecast doom, but inspire action and hope. Every life saved is a triumph of data and humanity working together.
Limits of Prediction: The Unpredictable Human Factor
No matter how sophisticated, algorithms can never predict every twist of fate. Accidents, acts of kindness, sudden recoveries—life is full of surprises that defy calculation. Even the best models are only as good as the data and assumptions they’re built on. Sometimes, real people defy the odds, living long past their predicted expiration date. These moments remind us that, at the end of the day, life is not just a series of numbers.
Children and Predictive Healthcare
The use of death-predicting algorithms in pediatric care raises unique ethical questions. Should parents be told if their child is at high risk? Will this knowledge help or haunt them? The emotional stakes are enormous, and the potential for harm is real. Algorithms might help doctors spot rare diseases or anticipate crises, but they can’t replace the love, intuition, and resilience that families bring to the fight for every child’s life.
Algorithmic Death: Science or Science Fiction?
The idea of a machine predicting your death feels pulled from a dystopian novel, yet it’s happening now in labs and clinics worldwide. As the technology improves, the line between science and science fiction blurs. Will we one day see death countdowns on our smartwatches? Or will society reject such tools as too cold, too invasive, or too fatalistic? The future is unfolding before our eyes, and the ending is anything but certain.
The Role of Consent and Choice

In this new era, the question of consent becomes urgent. Should patients be allowed to opt out of death predictions? How much say should you have in how your data is used? Informed consent must evolve to keep pace with the power—and risk—of predictive algorithms. Respecting people’s wishes, and ensuring they understand the implications, will be key to building a future where technology serves humanity, not the other way around.
Could Predictive Healthcare Change Our Relationship with Death?
As we hand more of our fate over to machines, our relationship with death itself may change. Will knowing our likely end make us braver, kinder, more focused on what matters? Or will it haunt us, casting a shadow over every joy? The answer will depend on how we use these tools—not to surrender to fate, but to live more fully in the time we have.
What would you do if you knew when your time would come?